Abstract
Purpose
To determine whether retrograde perfusion of cooled blood into one internal jugular vein (IJV) in the pig can selectively reduce the brain temperature without affecting the core body temperature (CBT).
Methods
In 7 domestic pigs, the left IJV was catheterized on one side and a catheter placed with the tip immediately below the rete mirabile. Thermistors were placed in both brain hemispheres and the brain temperature continuously registered. Thermistors placed in the rectum registered the CBT. From a catheter in the right femoral vein blood was aspirated with the aid of a roller pump, passed through a cooling device, and infused into the catheter in the left IJV at an initial rate of 200 ml/min.
Results
Immediately after the start of the infusion of cooled blood (13.8°C) into the IJV, the right brain temperature started to drop from its initial 37.9°C and reached 32°C within 5 min. By increasing the temperature of the perfusate a further drop in the brain temperature was avoided and the brain temperature could be kept around 32°C during the experiment. In 4 of the animals a heating blanket was sufficient to compensate for the slight drop in CBT during the cooling period.
Conclusions
We conclude that brain temperature can be reduced in the pig by retrograde perfusion of the internal jugular vein with cooled blood and that the core body temperature can be maintained with the aid of a heating blanket.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Profound and moderate hypothermia has been employed in cardiac, thoracic, and brain surgery, to protect the brain against damage during periods of ischemia caused by the surgical procedure. With the advent of animal models that allow long-term recovery, it was demonstrated that mild hypothermia (30–33°C) provides almost 100% protection if instituted prior to a transient episode of global cerebral ischemia [1], and up to 40% protection if hypothermia is instituted as late as 12 hr after an ischemic insult [2]. Hypothermia introduced in the post-ischemic phase was found to be most effective if the treatment persisted for 24 hr, and improved structural as well as neurologic outcome [3]. These successful preclinical studies initiated several clinical trials. Two have been completed, and enrolled 185 and 196 cardiac arrest patients in Australia and Europe, respectively. Both studies reported a 40–50% increase in favorable outcome after treatment with therapeutic hypothermia (32–34°C) [4, 5]. Also two feasibility studies employing therapeutic hypothermia have been conducted in stroke patients [6, 7]. In these studies endovascular cooling was used to lower whole-body and brain temperature, and a mean time to reach target temperature was 77 min.
Several problems are associated with whole-body cooling [8, 9]. Firstly, even if endovascular cooling is faster than external cooling using blankets, experimental stroke studies in rats show that hypothermia is effective only if initiated within 3 hr after middle cerebral artery occlusion. A faster cooling method is therefore warranted for application of therapeutic hypothermia to stroke patients. Secondly, whole-body cooling is associated with severe shivering. Hence, patients need to be anesthetized—with all the complications associated with this procedure in an elderly patient cohort. Thirdly, whole-body hypothermia increases incidents of hypotension, cardiac arrhythmias, hemorrhage and pneumonia. A cooling method specifically targeting the brain, ideally leaving the rest of the body normothermic, would be safer and not require intensive care.
Materials and Methods
Animals and Anesthesia
Seven Swedish domestic pigs with a mean body weight of 63 kg (range 60–72 kg) were used for the study. All animal experiments were approved by the ethics committee for animal studies at Lund University. The animals were fasted overnight with free access to water. All animals received premedication with intramuscular ketamine (Ketalar, Parke-Davis, NJ) 10 mg/kg body weight and xylazine (Rompun, Bayer, Gothenburg, Sweden) 0.2 mg/kg body weight. For anesthesia induction sodium thiopental (Pentotal, Abbot, North Chicago, IL) 5 mg/kg body weight and atropine (Atropine, Kabi Pharmacia, Uppsala, Sweden) 0.02 mg/kg body weight intravenously were used. Pancuronium (Pavulon, Organon Teknika, Boxel, The Netherlands) was given as a continuous intravenous infusion after tracheostomy and introduction of the tracheal tube (Portex #8, Hythe, UK) at a dose of 0.02 mg/kg per hour. During the experiment anesthesia was maintained using a mixture of 8 g ketamine and 300 mg pancuronium bromide dissolved in 5% glucose to 500 ml as a continuous infusion of 25 ml/hr. Volume-controlled ventilation was employed (Servo Ventilator 900A, Siemens Elema, Solna, Sweden) to maintain normal venous conditions (minute volume 150–200 ml/kg, 20 breaths/min, PEEP = 5 cm H2O, inspired oxygen fraction = 0.5). Euthanasia was induced by ventricular fibrillation with injection of potassium chloride (Fresenius Kabi, Uppsala, Sweden).
Procedures
The left carotid artery was used to place an arterial line into the aortic arch for pressure recording. Before the insertion the pressure-monitoring catheters were calibrated to atmospheric pressure at the level of the right atrium and intrathoracic aorta respectively. Temperatures were measured with thermistors in the rectum, inlet and outlet cooled blood, and cerebral cortex. The thermistors were placed bilaterally 1 cm down in the parietal cerebral cortex after trepanation. Ultrasonic flow probes (Transonic Flow Probe, Probe #35B 452) were placed around the right carotid artery and the inlet tubing from the cooling system. Blood samples were taken from the right atrium and the aortic arch and analyzed for blood gases, oxygen saturation, hemoglobin, and hematocrit to follow the condition of the animals. Through the cut down over the left internal jugular vein (IJV) a central venous line was placed in the right atrium and a 25 cm long 5 Fr catheter was introduced in the cranial direction into the same vein and advanced under fluoroscopic control to a position immediately below the rete mirabile. The position was confirmed by manual injection of contrast medium. The catheter was secured in position by a ligature around the vein. Through a cut down in the right groin a 9 Fr catheter was introduced into the femoral vein and advanced into the inferior vena cava (IVC).
In the first animal of the study no attempts were made to stabilize the body temperature. In the following two animals a 12 Fr double-lumen hemodialysis catheter (Cook Europe, Copenhagen, Denmark) was placed into the IVC via the left femoral vein. Aspirated blood from one lumen of this catheter was passed through a roller pump heating device (Jostra heater/cooler unit HCU, Jostra, Hechingen, Germany) and returned through the other lumen of the dialysis catheter to maintain the body temperature. The torso of the last four animals was wrapped with an electrical heating blanket for the same purpose.
The perfusion circuits were primed with 150 ml of lactated Ringer solution. A roller pump (HL20, Twin pump, Jostra, Hechingen, Germany) was chosen for the selective brain perfusion through the left IJV catheter. The pump was carefully calibrated according to the manufacturer’s instructions before each case. The catheter in the right femoral vein was connected to the roller pump. The pump flow was set to 200 ml/min at the start of the perfusion. Between the roller pump and its connection to the IJV catheter a cooler device (Sorin Dideco Cardioplegia Heatexchanger and Jostra heater/cooler unit, HCU) was positioned, and the temperature of the fluid entering the IJV catheter was continuously registered.
Results
Baseline registration of all parameters was performed prior to retrograde perfusion was started through the catheter in the IJV. Blood gases, oxygen saturation, hemoglobin and hematocrit did not show any adverse changes during the procedures, which were performed without any complications.
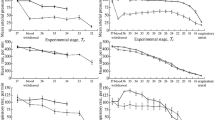
Temperature of the rectum (TR) was 38.5 ± 1.0°C, the temperature of the right brain (TRB) was 37.9 ± 0.9°C, and the temperature of the left brain (TLB) was 38.2 ± 0.9°C. The infusion into the IJV with the primed lactated Ringer solution was followed by blood chilled to 13.7 ± 1.8°C at a rate of 200 ml/min. Perfusion continued a this speed for 40–60 min. Brain temperature responded immediately on the cold perfusate (Fig. 1).
Temperature registration during selective cooling of a pig brain. Traces denote temperatures in the rectum (TR), the left brain (TLB), the right brain (TRB), and the perfusate (TP). The thin line indicates temperature and time from the start of the cooling procedure until target temperature (32°C) is reached.
In the first animal no attempts were made to maintain the body temperature, which fell from 37.3°C to 35.4°C over the duration of the experiment (42 min). In the following two animals heated blood was infused to compensate for the drop in body temperature. When body temperature showed a tendency to decrease, the double-lumen hemodialysis catheter was used to pump blood from the IVC with a roller pump, and then to heat the blood to 38°C and reinfuse it into the IVC. With this procedure the body temperature could be maintained at approximately 37°C. In the subsequent four experiments, the torso of the animal was wrapped in a heating blanket, which was sufficient to maintain the core body temperature approximately 37°C during the study.
After 5 min of perfusion the TRB was 32.7 ± 1.5°C, the TLB 32.0 ± 1.5°C, the TR 38.2 ± 0.7°C, and the temperature of the perfusate 13.0 ± 1.6°C (n = 7). As the brain temperature showed a tendency to fall below the desired level of 32°C the temperature of the perfused blood was slowly increased until after 10 min of perfusion the temperature of the perfusate was increased to 17.2 ± 2.1°C, that of the TRB was 32.0 ± 1.3°C, the TLB was 30.2 ± 1.4°C, and the TR was 37.9 ± 0.7°C. Twenty minutes after the start of the perfusion the TRB was 32.0 ± 1.2°C, the TLB was 32.7 ± 1.2°C, and the TR was 37.5 ± 0.9°C with a perfusion temperature of 20.4 ± 2.1°C (Fig. 2).
Discussion
Despite years of research no pharmacologic neuroprotective agent has been introduced into clinical practice to protect the brain against ischemic injury [8]. Mild whole-body hypothermia is currently the most effective measure taken to protect the brain against ischemic injury in the clinical setting, but it requires intensive care and is associated with risks and complications that may be unfavorable for the diseased and elderly patient [9, 10].
Here we have presented a method for rapid cooling of the pig brain while the rest of the body is kept at normothermic temperature (Figs. 1, 2). The method is fast in several aspects that are important for its applicability in the clinical setting, particularly following stroke and cardiac arrest. Firstly, placement of a balloon catheter in one IJV makes reversal of flow possible, and an extracorporeal cooling line can be established through extraction of blood from another vein (femoral or contralateral IJV). This can be performed within minutes after the arrival of the patient at the hospital. Secondly, once initiated the selective cooling of the brain is very quick. In addition, this method of selective cooling is favorable since it completely avoids the introduction of catheters into the arteries to the brain, thus minimizing the hazards of embolic complications. In addition, the moderate cooling of the whole body associated with the procedure can be compensated for by heating blankets. This could avoid complications of pneumonia and cardiac arrhythmias and hemorrhage. Furthermore, the risk of thrombosis is small since the cooling of the blood decreases the rate of thrombocyte aggregation, and the constant flow of fluid in the catheter should prevent clotting at the catheter tip.
Admittedly, the human brain does not possess a rete mirabile, but the brain arteries (carotid and vertebral) are in close proximity to the draining cerebral veins. In the pig, the common carotid artery gives rise to the ascending pharyngeal artery, which mostly corresponds to the human internal carotid artery (ICA). The ascending pharyngeal artery gives rise to the rete mirabile on the same side but communicates with the contralateral rete mirabile. The cerebral arteries originate from the arterial rete mirabile. The veins draining the brain in turn give rise to a venous rete mirabile, which drains into the IJV [11]. In man the ICA and the IJV are in close proximity within a sheath in the upper half of the neck. A venous network covers the ICA, and drains into the adjacent IJV. In the skull, the ICA passes through the cavernous sinus before it passes through the dura to form the proximal ophthalmic segment [12]. The spatial-anatomic relationship of the suboccipital cavernous sinus to the vertebral arteries is strikingly similar to that of the petrous-cavernous sinus to the ICA. The IJV has multiple communications to the suboccipital cavernous sinus [13]. Hence, the carotid and vertebral arteries are in close anatomic contact to the draining IJV, which would permit efficient heat exchange between these structures when the veins are perfused with cooled blood.
We can conclude that the method described could be useful for treatment of patients suffering from stroke, cardiac arrest, or other causes of brain ischemia.
References
Busto R, Dietrich WD, Globus MY, Valdes I, Scheinberg P, Ginsberg MD (1987) Small differences in intraischemic brain temperature critically determine the extent of ischemic neuronal injury. J Cereb Blood Flow Metab 7:729–738
Coimbra C, Boris-Moller F, Drake M, Wieloch T (1996) Diminished neuronal damage in the rat brain by late treatment with the antipyretic drug dipyrone or cooling following cerebral ischemia. Acta Neuropathol (Berl) 92:447–453
Colbourne F, Corbett D (1989) Delayed postischemic hypothermia: A six month survival study using behavioral and histological assessments of neuroprotection. J Neurosci 15:7250–7260
Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K (2002) Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 346:557–563
Hypothermia after Cardiac Arrest Study Group (2002) Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 346:549–556
De Georgia MA, Krieger DW, Abou-Chebl A, Devlin TG, Jauss M, Davis SM, Koroshetz WJ, Rordorf G, Warach S (2004) Cooling for Acute Ischemic Brain Damage (COOL AID): A feasibility trial of endovascular cooling. Neurology 63:312–317
Schwab S, Georgiadis D, Berrouschot J, Schellinger PD, Graffagnino C, Mayer SA (2001) Feasibility and safety of moderate hypothermia after massive hemispheric infarction. Stroke 32:2033–2035
Gladstone DJ, Black SE, Hakim AM; Heart, Stroke Foundation of Ontario Centre of Excellence in Stroke Recovery (2002) Toward wisdom from failure: Lessons from neuroprotective stroke trials. Stroke 33:2123–2136
Krieger DW, Yenari MA (2004) Therapeutic hypothermia for acute ischemic stroke: What do laboratory studies teach us? Stroke 35:1482–1489
Olsen TS, Weber UJ, Kammersgaard LP (2003) Therapeutic hypothermia for acute stroke. Lancet Neurol 2:410–416
Dondelinger RF, Ghysels MP, Brisbois D, Donkers E, Snaps FR, Saunders J, Devière J (1998) Relevant radiological anatomy of the pig as a training model in interventional radiology. Eur Radiol 8:1254–1273
Bouthillier A, van Loveren HR, Keller JT (1996) Segments of the internal carotid artery: A new classification. Neurosurgery 38:425–432
Arnautovic KI, al-Mefty O, Pait TG, Krisht AF, Husain MM (1997) The suboccipital cavernous sinus. J Neurosurg 86:252–262
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allers, M., Boris-Möller, F., Lunderquist, A. et al. A New Method of Selective, Rapid Cooling of the Brain: An Experimental Study. Cardiovasc Intervent Radiol 29, 260–263 (2006). https://doi.org/10.1007/s00270-004-0271-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-004-0271-6