Abstract
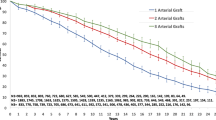
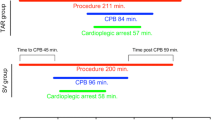
Total arterial myocardial revascularization (TAMR) is advisable because of the excellent long-term patency of arterial conduits. We present early and midterm outcomes of five different surgical configurations for TAMR. Between January 1998 and May 2004, 112 patients (aged 56.5 ± 4.5 years, 20% female) with three-vessel disease underwent TAMR. The internal mammary arteries (IMAs) were harvested in a sketelonized fashion. The surgical techniques for TAMR consisted in Y or T composite grafts (n = 88, 78%) constructed between the in situ right IMA (RIMA) and the free left IMA (LIMA) graft (n = 58) or the radial artery (n = 30) (RA) in three different configurations. The other techniques consisted in T- and inverted T-graft (n = 24, 22%) constructed between the RA conduit and the free LIMA graft in two different configurations. The mean follow-up time was 40 ± 23 months. Postoperative angiographic control was performed in 76/111 (70%) patients. Overall, 472 arterial anastomoses (average 4.2 per patient) were performed. One (0.9%) patient, undergoing the inverted T-graft technique, died on postoperative day 2. Another patient (0.9%), undergoing the λ-graft technique using both IMAs and RA, suffered a new myocardial infarction probably due to RA conduit vasospasm. One week after surgery, after the transthoracic echocardiographic Doppler with adenosine provocative test, the coronary flow reserve (CFR) at the LIMA and RIMA main stems were 2 ± 0.4 and 2.4 ± 0.3, respectively. At 12-month follow-up, after adenosine provocative test, the CFRs at the LIMA and RIMA stems were significantly higher than the values at 1 week after surgery within the same group; LIMACFR (1 week) 2.4 ± 0.3 (12 months) vs 2 ± 04 (1 week), P = 0.002; RIMACFR 2.58 ± 0.4 vs 2.4 ± 0.3, P = 0.001. The CFR at the RIMA main stem was higher in all measurements within the same group than in the LIMA main stem, but not significantly. In one patient undergoing the λ-graft technique using both IMAs, the RIMA was found to have a string sign. Postoperative angiography in 50 patients showed that the patency rate for the LIMA was 100%, for the RIMA 97.3%, and for the RA 96.7%. Angiography at 3-year follow-up in 76 patients documented excellent patency rates of the LIMA (97.4%), RIMA (95%), and RA (87%). Survival at 7 years was 92.5%, event-free survival 89.3%, and freedom from angina 94%. Total arterial myocardial revascularization using different surgical configurations is safe and effective. The use of composite arterial grafts provides excellent clinical and angiographic results, with a low rate of angina recurrence and late cardiac events. These configurations allow for complete arterial revascularization.
Similar content being viewed by others
References
JW Butany TE David M Ohja (1998) ArticleTitleHistological and morphometric analyses of early and late aortocoronary vein grafts and distal anastomoses Can J Cardiol 14 671–677 Occurrence Handle1:STN:280:DyaK1c3ptV2qsA%3D%3D Occurrence Handle9627522
Y Higuchi A Hirayama M Shimizu T Sakakibara K Kodama (2002) ArticleTitlePostoperative changes in angiographically normal saphenous vein coronary bypass grafts using intravascular ultrasound Heart Vessels 17 57–60 Occurrence Handle10.1007/s003800200044 Occurrence Handle12541095
DL Galbut EA Traad MJ Dorman (1990) ArticleTitleSeventeen-year experience with bilateral internal mammary grafts Ann Thorac Surg 49 195–201 Occurrence Handle1:STN:280:By%2BC28rlsFU%3D Occurrence Handle2306140
AN Calafiore G Di Giammarco N Luciani N Maddestra E Di Nardo R Angelini (1994) ArticleTitleComposite arterial conduits for a wider arterial myocardial revascularization Ann Thorac Surg 58 185–190 Occurrence Handle1:STN:280:ByuA3M7mslU%3D Occurrence Handle8037521
M Bonacchi E Prifti F Battaglia G Frati G Sani G Popoff (2003) ArticleTitleIn situ retrocaval skeletonized right internal thoracic artery anastomosed to the circumflex system via transverse sinus: technical aspects and postoperative outcome J Thorac Cardiovasc Surg 126 1302–1313 Occurrence Handle10.1016/S0022-5223(03)01277-7 Occurrence Handle14666000
TM Sundt Suffix3rd I-TB Barner CJ Camillo WA Gay SuffixJr (1999) ArticleTitleTotal arterial revascularization with an internal thoracic artery and radial artery T graft Ann Thorac Surg 68 399–404 Occurrence Handle10.1016/S0003-4975(99)00693-1 Occurrence Handle10475403
AM Calafiore GD Giammarco G Teodori (1995) ArticleTitleRadial artery and inferior epigastric artery in composite grafts Ann Thorac Surg 60 617–624 Occurrence Handle10.1016/0003-4975(95)00479-5
EL Jones OM Lattouf WS Weintraub (1989) ArticleTitleCatastrophic consequences of internal mammary artery bypass hypoperfusion J Thorac Cardiovasc Surg 98 902–907 Occurrence Handle1:STN:280:By%2BD2c3ks1Y%3D Occurrence Handle2572732
GW He TE Acuff WH Ryan MJ Mack (1994) ArticleTitleRisk factors for operative mortality in elderly patients undergoing internal mammary artery grafting Ann Thorac Surg 57 IssueID6 1453–1460 Occurrence Handle1:STN:280:ByuB1c%2FitFA%3D Occurrence Handle7912063
M Bonacchi E Prifti G Frati M Leacche A Salica G Giunti P Proietti B Furci F Miraldi (1999) ArticleTitleTotal arterial myocardial revascularization using new composite graft techniques for internal mammary and/or radial arteries conduits J Card Surg 14 408–416 Occurrence Handle1:STN:280:DC%2BD3cvmsFCgug%3D%3D Occurrence Handle11021365
M Bonacchi E Prifti G Giunti A Salica (2000) ArticleTitleRight Y-graft, a new surgical technique using mammary arteries for total myocardial revascularization Ann Thorac Surg 70 820–823 Occurrence Handle10.1016/S0003-4975(00)01500-9 Occurrence Handle1:STN:280:DC%2BD3cvmtlCrtA%3D%3D Occurrence Handle11016316
M Bonacchi E Prifti G Giunti G Frati (2001) ArticleTitleRestoration of patency after apparent occlusion of the λ-graft's right branch Heart Vessels 16 20–22 Occurrence Handle10.1007/s003800170004 Occurrence Handle1:STN:280:DC%2BD38%2FpvVOgtA%3D%3D Occurrence Handle11829214
J Tatoulis BF Buxton JA Fuller AG Royse (1999) ArticleTitleTotal arterial coronary revascularization: techniques and results in 3 220 patients Ann Thorac Surg 68 2093–2099 Occurrence Handle1:STN:280:DC%2BD3c%2FotlaksQ%3D%3D Occurrence Handle10616983
AJ Tector DC Kress FX Downey TM Schmahl (1996) ArticleTitleComplete revascularization with internal thoracic artery grafts Semin Thorac Cardiovasc Surg 8 29–41 Occurrence Handle1:STN:280:BymB2s3ntF0%3D Occurrence Handle8679748
AA Pitsis HC Cullen F Musumeci AC Zaman EG Butchart (1999) ArticleTitleA new strategy of total revascularization Ann Thorac Surg 67 1186–1187 Occurrence Handle10.1016/S0003-4975(99)00102-2 Occurrence Handle1:STN:280:DyaK1M3lt1Sgtg%3D%3D Occurrence Handle10320286
AM Calafiore G Vitolla A Taco C Fino G Di Giammarco F Marchesani G Teodori G D'Addario V Mazzei (1999) ArticleTitleBilateral internal mammary artery grafting: midterm results of pedicled versus skeletonized conduits Ann Thorac Surg 67 1637–1642 Occurrence Handle1:STN:280:DyaK1MzhvVWmsw%3D%3D Occurrence Handle10391267
T Tashiro K Nakamura A Iwakuma R Zaitu H Iwahashi A Murai M Kimura (1999) ArticleTitleInverted T graft: novel technique using composite radial and internal thoracic arteries Ann Thorac Surg 67 629–631 Occurrence Handle10.1016/S0003-4975(98)01240-5 Occurrence Handle1:STN:280:DyaK1M3jtVSguw%3D%3D Occurrence Handle10215200
J Gurevitch Y Paz I Shapira M Matsa A Kramer D Pevni O Lev-Ran Y Moshkovitz R Mohr (1999) ArticleTitleRoutine use of bilateral skeletonized internal mammary arteries for myocardial revascularization Ann Thorac Surg 68 406–412 Occurrence Handle10.1016/S0003-4975(99)00460-9 Occurrence Handle1:STN:280:DyaK1Mvgt1eruw%3D%3D Occurrence Handle10475404
O Wendler B Hennen T Markwirth J Konig D Tscholl Q Huang E Shahangi HJ Schafers (1999) ArticleTitleT grafts with the right internal thoracic artery to left internal thoracic artery versus the left internal thoracic artery and radial artery: flow dynamics in the internal thoracic artery main stem J Thorac Cardiovasc Surg 118 841–848 Occurrence Handle1:STN:280:DC%2BD3c%2Fgs1Snuw%3D%3D Occurrence Handle10534689
AJ Tector S Amundsen TM Schmahl DC Kress M Peter (1994) ArticleTitleTotal revascularization with T grafts Ann Thorac Surg 57 33–39 Occurrence Handle1:STN:280:ByuC3cjgs1c%3D Occurrence Handle7904146
LR Sauvage HD Wu TE Kowalsky (1986) ArticleTitleHealing basis and surgical techniques for complete revascularization of the left ventricle using only the internal mammary arteries Ann Thorac Surg 42 449–465 Occurrence Handle1:STN:280:BiiD38votlw%3D Occurrence Handle3490233
HB Barner TM Sundt M Bailey Y Zang (2001) ArticleTitleMidterm results of complete arterial revascularization in more than 1000 patients using an internal thoracic artery/radial artery T graft Ann Surg 234 447–453 Occurrence Handle10.1097/00000658-200110000-00004 Occurrence Handle1:STN:280:DC%2BD3MrmslOmsA%3D%3D Occurrence Handle11573038
AW Pick TA Orszulak BJ Anderson HV Schaff (1997) ArticleTitleSingle versus bilateral internal mammary artery grafts: ten-year analysis Ann Thorac Surg 64 599–605 Occurrence Handle10.1016/S0003-4975(97)00620-6 Occurrence Handle1:STN:280:ByiH2M3msFA%3D Occurrence Handle9307445
MA Paz J Lupon X Bosch JL Pomar G Sanz (1993) ArticleTitlePredictors of early saphenous vein aortocoronary bypass occlusion Ann Thorac Surg 56 1101–1106 Occurrence Handle1:STN:280:ByuD2MfktFI%3D Occurrence Handle8239808
C Muneretto G Bisleri A Negri J Manfredi M Metra S Nodari L Culot L Dei Cas (2003) ArticleTitleTotal arterial myocardial revascularization with composite grafts improves results of coronary surgery in elderly: a prospective randomized comparison with conventional coronary artery bypass surgery Circulation 108 IssueIDSuppl 1 II29–II33 Occurrence Handle12970204
E Verhelst PY Etienne G El Khoury P Noirhomme J Rubay R Dion (1996) ArticleTitleFree internal mammary artery graft in myocardial revascularization Cardiovasc Surg 4 212–216 Occurrence Handle1:STN:280:ByiD3MvmtVM%3D Occurrence Handle8861440
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonacchi, M., Prifti, E., Maiani, M. et al. Perioperative and clinical-angiographic late outcome of total arterial myocardial revascularization according to different composite original graft techniques. Heart Vessels 21, 69–77 (2006). https://doi.org/10.1007/s00380-005-0856-2
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00380-005-0856-2