Abstract
Background
Artificial intelligence and computer vision have revolutionized laparoscopic surgical video analysis. However, there is no multi-center study focused on deep learning-based laparoscopic cholecystectomy phases recognizing. This work aims to apply artificial intelligence in recognizing and analyzing phases in laparoscopic cholecystectomy videos from multiple centers.
Methods
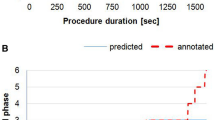
This observational cohort-study included 163 laparoscopic cholecystectomy videos collected from four medical centers. Videos were labeled by surgeons and a deep-learning model was developed based on 90 videos. Thereafter, the performance of the model was tested in additional ten videos by comparing it with the annotated ground truth of the surgeon. Deep-learning models were trained to identify laparoscopic cholecystectomy phases. The performance of models was measured using precision, recall, F1 score, and overall accuracy. With a high overall accuracy of the model, additional 63 videos as an analysis set were analyzed by the model to identify different phases.
Results
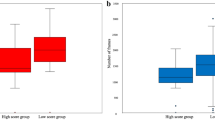
Mean concordance correlation coefficient for annotations of the surgeons across all operative phases was 92.38%. Also, the overall phase recognition accuracy of laparoscopic cholecystectomy by the model was 91.05%. In the analysis set, there was an average surgery time of 2195 ± 896 s, with a huge individual variance of different surgical phases. Notably, laparoscopic cholecystectomy in acute cholecystitis cases had prolonged overall durations, and the surgeon would spend more time in mobilizing the hepatocystic triangle phase.
Conclusion
A deep-learning model based on multiple centers data can identify phases of laparoscopic cholecystectomy with a high degree of accuracy. With continued refinements, artificial intelligence could be utilized in huge data surgery analysis to achieve clinically relevant future applications.



Similar content being viewed by others
References
Hashimoto DA, Rosman G, Rus D, Meireles OR (2018) Artificial intelligence in surgery: promises and perils. Ann Surg 268:70–76
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, Thrun S (2017) Dermatologist-level classification of skin cancer with deep neural networks. Nature 542:115–118
Zappella L, Bejar B, Hager G, Vidal R (2013) Surgical gesture classification from video and kinematic data. Med Image Anal 17:732–745
Twinanda AP, Shehata S, Mutter D, Marescaux J, de Mathelin M, Padoy N (2017) EndoNet: a deep architecture for recognition tasks on laparoscopic videos. IEEE Trans Med Imaging 36:86–97
Hashimoto DA, Rosman G, Witkowski ER, Stafford C, Navarette-Welton AJ, Rattner DW, Lillemoe KD, Rus DL, Meireles OR (2019) Computer vision analysis of intraoperative video: automated recognition of operative steps in laparoscopic sleeve gastrectomy. Ann Surg 270:414–421
Morita S, Tabuchi H, Masumoto H, Yamauchi T, Kamiura N (2019) Real-time extraction of important surgical phases in cataract surgery videos. Sci Rep 9:16590
Dergachyova O, Bouget D, Huaulme A, Morandi X, Jannin P (2016) Automatic data-driven real-time segmentation and recognition of surgical workflow. Int J Comput Assist Radiol Surg 11:1081–1089
Jin Y, Dou Q, Chen H, Yu L, Qin J, Fu CW, Heng PA (2018) SV-RCNet: workflow recognition from surgical videos using recurrent convolutional network. IEEE Trans Med Imaging 37:1114–1126
Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, Endo I, Umezawa A, Asai K, Suzuki K, Mori Y, Okamoto K, Pitt HA, Han HS, Hwang TL, Yoon YS, Yoon DS, Choi IS, Huang WS, Gimenez ME, Garden OJ, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan ACW, Lau WY, Liu KH, Su CH, Misawa T, Nakamura M, Horiguchi A, Tagaya N, Fujioka S, Higuchi R, Shikata S, Noguchi Y, Ukai T, Yokoe M, Cherqui D, Honda G, Sugioka A, de Santibanes E, Supe AN, Tokumura H, Kimura T, Yoshida M, Mayumi T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M (2018) Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25:73–86
Iwashita Y, Ohyama T, Honda G, Hibi T, Yoshida M, Miura F, Takada T, Han HS, Hwang TL, Shinya S, Suzuki K, Umezawa A, Yoon YS, Choi IS, Huang WS, Chen KH, Watanabe M, Abe Y, Misawa T, Nagakawa Y, Yoon DS, Jang JY, Yu HC, Ahn KS, Kim SC, Song IS, Kim JH, Yun SS, Choi SH, Jan YY, Sheen-Chen SM, Shan YS, Ker CG, Chan DC, Lee KT, Toyota N, Higuchi R, Nakamura Y, Mizuguchi Y, Takeda Y, Ito M, Norimizu S, Yamada S, Matsumura N, Shindoh J, Sunagawa H, Hasegawa H, Rikiyama T, Sata N, Kano N, Kitano S, Tokumura H, Yamashita Y, Watanabe G, Nakagawa K, Kimura T, Yamakawa T, Wakabayashi G, Endo I, Miyazaki M, Yamamoto M (2016) What are the appropriate indicators of surgical difficulty during laparoscopic cholecystectomy? Results from a Japan–Korea–Taiwan multinational survey. J Hepatobiliary Pancreat Sci 23:533–547
Kitaguchi D, Takeshita N, Matsuzaki H, Takano H, Owada Y, Enomoto T, Oda T, Miura H, Yamanashi T, Watanabe M, Sato D, Sugomori Y, Hara S, Ito M (2019) Real-time automatic surgical phase recognition in laparoscopic sigmoidectomy using the convolutional neural network-based deep learning approach. Surg Endosc 34:4924
Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Gimenez ME, de Santibanes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M (2018) Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25:41–54
Meeuwsen FC, van Luyn F, Blikkendaal MD, Jansen FW, van den Dobbelsteen JJ (2019) Surgical phase modelling in minimal invasive surgery. Surg Endosc 33:1426–1432
Kannan S, Yengera G, Mutter D, Marescaux J, Padoy N (2020) Future-state predicting LSTM for early surgery type recognition. IEEE Trans Med Imaging 39:556–566
Gutt CN, Encke J, Koninger J, Harnoss JC, Weigand K, Kipfmuller K, Schunter O, Gotze T, Golling MT, Menges M, Klar E, Feilhauer K, Zoller WG, Ridwelski K, Ackmann S, Baron A, Schon MR, Seitz HK, Daniel D, Stremmel W, Buchler MW (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg 258:385–393
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211:132–138
Strasberg SM (2019) A three-step conceptual roadmap for avoiding bile duct injury in laparoscopic cholecystectomy: an invited perspective review. J Hepatobiliary Pancreat Sci 26:123–127
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Gouma DJ, Garden OJ, Buchler MW, Kiriyama S, Kimura Y, Tsuyuguchi T, Itoi T, Yoshida M, Miura F, Yamashita Y, Okamoto K, Gabata T, Hata J, Higuchi R, Windsor JA, Bornman PC, Fan ST, Singh H, de Santibanes E, Kusachi S, Murata A, Chen XP, Jagannath P, Lee S, Padbury R, Chen MF, Tokyo Guidelines Revision C (2012) New diagnostic criteria and severity assessment of acute cholecystitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 19:578–585
Huang L, Li TJ (2018) Laparoscopic surgery for gastric cancer: where are we now and where are we going? Expert Rev Anticancer Ther 18:1145–1157
Palter VN, Grantcharov TP (2012) A prospective study demonstrating the reliability and validity of two procedure-specific evaluation tools to assess operative competence in laparoscopic colorectal surgery. Surg Endosc 26:2489–2503
De Siqueira JR, Gough MJ (2016) Correlation between experience targets and competence for general surgery certification. Br J Surg 103:921–927
Langerman A, Grantcharov TP (2017) Are we ready for our close-up?: why and how we must embrace video in the OR. Ann Surg 266:934–936
Hu YY, Mazer LM, Yule SJ, Arriaga AF, Greenberg CC, Lipsitz SR, Gawande AA, Smink DS (2017) Complementing operating room teaching with video-based coaching. JAMA Surg 152:318–325
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Heniford BT, Scott DJ (2007) Closing the gap in operative performance between novices and experts: does harder mean better for laparoscopic simulator training? J Am Coll Surg 205:307–313
Curtis NJ, Foster JD, Miskovic D, Brown CSB, Hewett PJ, Abbott S, Hanna GB, Stevenson ARL, Francis NK (2020) Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg 155:590
Tang B, Hanna GB, Carter F, Adamson GD, Martindale JP, Cuschieri A (2006) Competence assessment of laparoscopic operative and cognitive skills: objective structured clinical examination (OSCE) or observational clinical human reliability assessment (OCHRA). World J Surg 30:527–534
Foster JD, Miskovic D, Allison AS, Conti JA, Ockrim J, Cooper EJ, Hanna GB, Francis NK (2016) Application of objective clinical human reliability analysis (OCHRA) in assessment of technical performance in laparoscopic rectal cancer surgery. Tech Coloproctol 20:361–367
Pugh CM, Hashimoto DA, Korndorffer JR Jr (2020) The what? How? And who? Of video based assessment. Am J Surg 221:13
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJ, Michigan Bariatric Surgery C (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Acknowledgements
We are thankful to the contribution that all of the authors have made.
Funding
This work is supported by key project of Health Commission of Sichuan Province, China (20ZD003).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
Dr. Ke Cheng, Dr. Jiaying You, Dr. Shangdi Wu, Dr. Zixin Chen, Dr. Zijian Zhou, Mr. Jingye Guan, Prof. Bing Peng and Dr. Xin Wang have no conflict of interest or financial ties to disclose. This work is supported by key project of Health Commission of Sichuan Province, China (20ZD003).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, K., You, J., Wu, S. et al. Artificial intelligence-based automated laparoscopic cholecystectomy surgical phase recognition and analysis. Surg Endosc 36, 3160–3168 (2022). https://doi.org/10.1007/s00464-021-08619-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08619-3