Abstract
This paper investigates the effects of global budgets on the amount of resources devoted to cardio-cerebrovascular disease patients by hospitals of different ownership types and these patients’ outcomes. Theoretical models predict that hospitals have financial incentives to increase the quantity of treatments applied to patients. This is especially true for for-profit hospitals. If that’s the case, it is important to examine whether the increase in treatment quantity is translated into better treatment outcomes. Our analyses take advantage of the National Health Insurance of Taiwan’s implementation of global budgets for hospitals in 2002. Our data come from the National Health Insurance’s claim records, covering the universe of hospitalized patients suffering acute myocardial infarction, ischemic heart disease, hemorrhagic stroke, and ischemic stroke. Regression analyses are carried out separately for government, private not-for-profit and for-profit hospitals. We find that for-profit hospitals and private not-for-profit hospitals did increase their treatment intensity for cardio-cerebrovascular disease patients after the 2002 implementation of global budgets. However, this was not accompanied by an improvement in these patients’ mortality rates. This reveals a waste of medical resources and implies that aggregate expenditure caps should be supplemented by other designs to prevent resources misallocation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This study investigates the impact of global budgeting on the treatment intensity and patients’ outcomes. In developed or high income countries, governments play an important role in financing health care services through the public provision of health insurance or direct provision of health care services, or through subsidizing the utilization of medical services (see Docteur and Oxley 2004). Thus, the rapid increase in health care expenditure since the 1960s has become a great concern to policy makers in these countries. In response to soaring health care costs, various cost containment measures have been implemented. Examples of cost containment measures include capitation, DRG-based payment method and global budgeting. According to Le Grand (2003), among different cost containment measures, global budgeting is the most effective one. Because global budgeting is effective in controlling medical expenditures, it is widely adopted in OECD countries (see Docteur and Oxley 2004; Wolfe and Moran 1993).
In the literature, there are numerous studies comparing patients’ outcomes under different payment systems: fee-for-service, capitation and DRG-based payment systems (see Christianson and Conrad 2011, for a recent review). However, even though there are studies on global budgets’ effects on the quantity of services supplied and the cost containment effectiveness, the literature is silent on the issue relating to patients’ welfare.Footnote 1 While global budgeting aims at curbing the growth in health care expenditure and it is shown to be effective in doing so, it is unclear whether successful cost containment is at the expense of patients’ welfare. If medical cost containment by global budgeting is accompanied by a decrease in patients’ welfare arising from worsening treatment outcomes, then the health authority should consider alternative cost containment methods or complemental measures to minimize this collateral damage. Alternatively, if the implementation of global budgets leads to an increase in treatment intensity, while treatment outcomes do not improve, there is a misallocation or a waste of medical resources and the use of global budgets as a containment device should be reconsidered.
The data we use come from the National Health Insurance (NHI hereafter) claim records, which is maintained and distributed by Taiwan’s National Health Research Institute. Our data cover the period January 2001– March 2003, and consist of administrative records of all patients suffering from AMI (acute myocardial infarction, ICD code: 410), ischemic heart disease (ICD code: 411–414), hemorrhagic stroke (ICD code: 434), and ischemic stroke (ICD code: 430–431) in that period. We use the total number of points, which is a unit measuring the quantity of service performed and is to be explained below, that a hospital claims for treating a patient as a measure of treatment intensity. For treatment outcomes, we use patient’s 30-day mortality as a proxy.
In our empirical analysis, we look at the changes in treatment intensity and outcomes of private for-profit, not-for-profit, and government hospitals separately. This is because findings obtained by previous studies show that the behaviors of for-profit, private not-for-profit, and government hospitals are likely to be very different probably due to the differences in their objective functions and constraints (e.g., tax exemptions and organizational structure). Especially, these findings imply that for-profit hospitals are more responsive to financial incentives. It is expected that for-profit hospitals are more responsive than not-for-profit hospitals to the launch of global budgets. For not-for-profit hospitals, since profit making is not their utmost concern, relative to for-profit hospitals their responses to global budgeting are likely to be sluggish.
Our empirical results suggest that after the launch of global budgets patients in for-profit and private not-for-profit hospitals received more treatments, while the quantity of services received by government hospitals’ patients did not change. However, there was no discernible improvement in the mortality rates of for-profit and private not-for-profit hospitals’ patients. This implies that there may be a waste of resources and a modification of the design of the global budget system may lead to an improvement in resource allocation.
Literature review
Different payment systems create different incentives to medical service providers. The responses of providers to these incentives in terms of service quantities and quality have important implications on patients’ treatment outcomes. It is generally agreed that under fee for-service providers have incentives to over-supply services. However, even though patients may receive more treatments, these treatments may be unnecessary or inappropriate. Thus, patients’ outcomes may not be better under fee-for-service.
To contain costs and improve health service quality, some insurance systems have adopted capitation or the DRG-based prospective payment systems. Providers are likely to limit the supply of services under these prospective payment systems (see Miller 2009, for a discussion). While prospective payment systems are found to succeed in containing medical cost, findings on its effects on patients’ outcomes are mixed even within a single study. For example, the results in Rogers et al. (1990) show that with the introduction of a DRG-based payment system while mortality following hospitalization is unaffected, patients are more likely to be discharged prematurely. Moreover, findings of Louis et al. (1999) suggest that even though service utilization declined with the replacement of a global budget system by a DRG-based payment system in Italy, patients’ in-hospital mortality rate was unaffected. Similar findings are obtained by Cheng et al. (2012) for the case of Taiwan, where a DRG-based payment system is introduced on top of a global budget system. By contrast, Cutler (1995) finds that the replacement of a cost-based reimbursement method by a diagnosis-based prospective payment system in the U.S. had adverse effects on patients’ outcomes.
Even though global budgeting is widely adopted as a medical cost containment measure, its economic implications are not well explored in the literature. Moreover, most theoretical studies on the subject focus mainly on the behavioral response of providers. Their results imply that, if the medical market is competitive, a larger quantity of medical services is provided under a global budget system, while a smaller amount of services is provided if providers have market power. Furthermore, there are different possible reasons suggesting that private not-for-profit and government medical service providers are insensitive to financial incentives, suggesting that they are less responsive to the launch of global budgets than for-profit providers. Below is a brief review of the relevant theoretical and empirical literature.
Among theoretical studies on global budgeting, an early study of the consequences of global budget as a cost containment device is Fan et al. (1998), whose results show that, given the same amount of medical expenditure, providers will provide a larger quantity of services under a global budget system if there is a large number of providers and they act competitively (i.e., do not coordinate with each other). If providers do coordinate, the results depend on the penalty imposed by the government for services supplied beyond the quota under the expenditure target system. These predictions are supported by their experimental results. Providers’ behavior under the global budget system and fee-for-service payment system in a competitive medical care market is analyzed by Benstetter and Wambach (2006). It is shown that under a global budget system the quantity of services supplied by a profit seeking provider depends on the expected price, which in turn depends on the aggregate quantity of services supplied by all providers in the system. They explain that the low price equilibrium, where providers supply a large quantity of services, is likely to be attained.
By contrast, Mougeot and Naegelen’s (2005) results suggest that compared with a fee-for-service payment system, an expenditure cap results in a lower level of service quality, implying a lower level of equilibrium quantity of services provided and social welfare. These results prevails in monopolistic as well as Cournot-competitive markets. It is likely that the difference in Mougeot and Naegelen’s (2005) results from others reviewed above is due to their assumptions that the government behaves strategically and providers choose the levels of service quality and cost-minimization effort to maximize profit. On the contrary, other studies assume that providers choose the quantity services to maximize profits.
Service providers in the theoretical studies reviewed above are assumed to be profit maximizing (e.g., they are for-profit providers). However, for-profit providers’ behavior are very likely to be different from that of private not-for-profit or public providers, which are subject to different institutional and financial constraints (see Sloan 2000). There are several possible reasons why private not-for-profit and public providers behave differently from their for-profit counterparts. Firstly, while both not-for-profit and public providers are not allowed to distribute profits, public providers are subject to additional political and legal constraints, e.g., regulations on government employee compensation and public opinion on the prices charged by public providers (see Hansmann 1980, and Wilson 1989). These constraints are likely to stifle not-for-profit and public providers’ response to financial incentives.
Secondly, private not-for-profit and public providers may have been founded for the purpose of serving a certain group of individuals or achieving certain objectives, e.g., philanthropy (see Weisbrod 1977). That is, profit maximization is not their first priority. Furthermore, the soft budget constraint of not-for-profit and public providers also suggests that they are less responsive to financial incentives (see Kornai 1986; Kornai et al. 2003, and Kornai 2009). Having a soft budget constraint implies that an organization is not allowed to fail even though it is making chronic losses and its subsidies will be offset by profits.
These theoretical studies’ predictions on the differences in hospital behavior due to differences in ownership are mostly borne out in findings of empirical studies. Previous studies find that, relative to their for-profit counterparts, private not-for-profit and public providers are sluggish in responding to financial incentives, and public providers are the least responsive (see, Duggan 2000; Sloan et al. 2001; Silverman and Skinner 2004; Horwitz 2005; Dafny 2005; Horwitz and Nichols 2009; Shen and Eggleston 2009). In addition, hospitals’ quality of care or treatment outcomes varies with their ownership (see McClellan and Staiger 2000; Eggleston et al. 2008; Lien et al. 2008). There are no empirical studies focusing on the differential responses of hospitals of different ownership to changes in the payment system.
There is several empirical research on hospital responses to global budgeting in term of quantities and quality of care. In general, findings of empirical studies support the prediction that the launch of global budgets leads to an increase in the quantity of medical services supplied. For example, in response to an expenditure cap, physicians in Quebec increased their activity levels, and provide more complex and high-priced procedures (see Rochaix 1993). Similarly, the study of Hurley et al. (1997) suggest that expenditure cap in Canada led to an increase in expenditure. In response to a global budget, dentists in Taiwan exhibit similar behavior (see Lee and Jones 2004). Also, hospitals in Taiwan are more likely to hospitalize patients under global budgeting, see, e.g., Chen et al. (2007), Cheng et al. (2009).
Few studies, except those by Tung and Chang (2010) and Chang et al. (2011), analyze the effect of global budgeting on the quality of care. Using 1997–2008 patient-level data extracted from the Taiwan’s NHI database, Tung and Chang (2010) and Chang et al. (2011) provide evidence that the adoption of global budgeting in 2002 had an adverse effect on the mortality of hospitalized patients suffering from stroke and AMI, respectively. However, their empirical results may be confounded by changes in the payment scheme implemented during their sample period.
To summarize, previous studies’ empirical and theoretical results suggest that (a) profit maximizing providers are likely to increase the quantity of service supplied, and (b) private not-for-profit and, especially, public providers are less responsive to profitable opportunities. Based on these findings, it can be conjectured that, while providers will increase the quantity of service supplied in response to the launch of global budgets, private not-for-profit and public providers are less responsive than their for-profit counterparts.
Background
National Health Insurance and hospital global budgets in Taiwan
Since March 1995, NHI provides insurance coverage to all residents in Taiwan. The medical benefits of Taiwan’s NHI are comprehensive, covering inpatient care, ambulatory care, emergency care, laboratory testing, diagnostic imaging, prescription, certain over-the-counter medicines, dental care, Chinese medicines, preventive care (e.g., pediatric immunization and adult health examination), etc. Taiwan’s NHI has substantially reduced the out-of-pocket expenditure of medical service utilization. For example, to see the doctor at a community clinic, a patient pays an appointment fee of NT$100 and a copayment of NT$50, which are equivalent to US$3.46 and US$1.73, respectively, at the March 1995 exchange rate.
Over ninety percent of hospitals in Taiwan are contracted NHI medical service providers. Initially, NHI contracted providers are reimbursed on a fee-for-service (FFS) basis. Under this payment system, a provider is credited a certain number of points for each treatment procedure offered and each point is worth NT$1 (approximately US$0.032 at the 2002 exchange rate).
The low out-of-pocket user costs under NHI allow liberal use of medical services by the general public. The FFS payment system also encouraged medical service providers to provide as much service as possible. This has led to a rapid growth in health care expenditure and the NHI system has incurred a huge deficit. Over the six year period 1996–2001, on average the annual growth rate of expenditure incurred by the NHI system was 7.43 % (where the average inflation rate is 1.18 %), and the NHI system accumulated a deficit of NT$12.82 billion. This has cast doubt on the long-term financial sustainability of the system, and eventually global budgets were installed to contain the rising health care expenditure. Global budgeting was used for dental services starting from 1998. This was followed by global budgets for Chinese Medicine in 2000, and community clinics in 2001.
Global budgets for all hospital services were set in place in July of 2002. The national budget for a given year is determined before the end of the previous year by consultation between the Bureau of National Health Insurance (BNHI) and hospital representatives. The aggregate level of expenditure in the previous year and age structure of the population determine the size of the national budgets. Moreover, the national budgets were divided into quarterly sub-budgets, with the relative size of the quarterly budgets determined by the actual quarterly expenditure in the previous years. Starting from 2003 regional budgets were introduced.
Each region’s share of a budget is determined by two factors: (a) the total medical expenditures claimed in the region in the previous year and (b) demographic characteristics (e.g., total population size, sex ratio, age structure, and the mortality rates). As such, while a provider’s current behavior has some effect on a region’s future expenditure cap, the effect is very small given that all regions are competitive and demographic factors carry a heavier weight in determining a region’s budget. See Table 1 for the counties/cities covered, and hospital market and demographic characteristics of the six regions.
Like the pre-global budget era, each hospital is offered a certain number of points for a service item. However, the point value (i.e., the amount of money that a hospital is reimbursed for each point earned) is uncertain, depending on the total volume of services provided by hospitals in that medical region. A region’s quarter \(q \) point value is determined as follows
The hospital budgets include inpatient and outpatient services. The global budget system does not apply to home care, mental health rehabilitation, and health care arising from disasters. Extra funding is provided to cover such expenditure. In addition, the point value for drugs and medication services, and preventive care is fixed at NT$1.
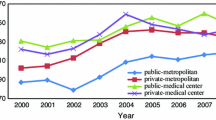
Global budgeting is effective in containing health care costs. Over the period 2002–2007, the average growth in the health care expenditure incurred by the NHI is 4.82 %, while the average inflation rate is 0.97 %, in contrast to 7.43 % for the period 1996–2001. Since service quantity has increased substantially, while expenditure is allowed to grow at a controlled rate, there is a decrease in point value, as showed in Fig. 1.
It is noted that in 2003 there was a jump in the point value and there was no fluctuation in point value across quarters. This is because during the 4 months of SARS epidemic (April–July, 2003) there was a shortfall in patient visits and a huge jump in hospitals’ nonreimbursible expenses to combat SARS, especially for large-scale hospitals. Some hospitals thus incurred heavy financial losses. In order to assist these hospitals, in addition to providing subsidies, in 2004 the BNHI abolished the quarterly budgets. Quarterly budgets were replaced by annual ones, such that each region’s 2003 reimbursement was based on a single point value for the whole year.
Point value. Data obtained from the Bureau of National Health Insurance: http://www.mohw.gov.tw/cht/DOS/Statistic_P.aspx?f_list_no=312&fod_list_no=1819&doc_no=4059
In view of the surge in the volume of health care services and deterioration in service quality accompanied by the hospital global budget system, in January 2004 the BNHI introduced the “Hospital Self-Management” scheme for selected hospitals, which are usually large. Participation in the scheme is by application and is subject to approval. A participating hospital has its own expenditure caps, which are negotiated between the hospital and the BNHI, and the point value of its services may be different from that of other hospitals. Furthermore, a participating hospital should have plans to improve its service quality. The “Hospital Self-Management” scheme was replaced by the “Hospital Excellence” scheme in July 2004. Under this scheme, there is more room for a participating hospital to negotiate the expenditure cap. In return, it has to follow stricter rules and has to draw up service quality improvement plans, which are subject to evaluation, and release its financial statements to the BNHI. Out of a total of 556 hospitals, there were 230 participating in the scheme in 2004. This study will focus on the period prior to the SARS epidemic and the introduction of the “Hospital Self-Management” scheme.
For-profit, private not-for-profit, and Government Hospitals in Taiwan
In Taiwan, hospitals can be broadly classified into three types: for-profit, private not-for-profit, and government hospitals. Separate analysis is carried out for these three types of hospitals due to their possible different responsiveness to the launch to global budgets. Below is a brief description of the hospital markets in Taiwan with respect to these three types of hospitals.
The establishment and operation of hospitals in Taiwan are governed by its Medical Law. According to this law, for-profit hospitals are established and run by physicians. Government hospitals are owned and operated by government agencies, local governments, or public universities. Private not-for-profit hospitals are owned by private not-for-profit corporations, e.g., private universities, religious corporations, and charitable organizations, which may be partially supported by private donations. A hospital run by a not-for-profit corporation is controlled by a board. It enjoys property tax exemption, and profit tax exemption if over 80 % of its earnings are spent.
Table 1 exhibits the numbers of different types of hospitals for the period 2001–2003. There are far more for-profit hospitals than private not-for-profit or government hospitals. Table 1 shows that in terms of hospital beds, for-profit hospitals are much smaller than their private not-for-profit and government counterparts. Moreover, as suggested by the Herfindahl index in Table 1 the hospital markets are competitive with most regions’ Herfindahl index being below 0.1 and the highest being 0.12 (i.e., region 6).
Data
Our data consist of National Health Insurance claim records of patients hospitalized during the period January 2001 and March 31, 2003. These records are maintained and distributed by Taiwan’s National Health Research Institute (NHRI). Our empirical analysis employs every single record of patients hospitalized due to AMI, ischemic heart disease, hemorrhagic stroke, and ischemic stroke during the sample period. In our sample there are totally 275,669 patients, and 29,615, 139,708, 79,836, and 28,487 patients, respectively, suffering from these four diseases.
Our rationale behind focusing on the four diseases is that they are the leading causes of mortality in Taiwan and their total treatment expenditure accounts for a large share of health care expenditures.Footnote 2 Another reason is that their onset is usually sudden and rapid such that a patient is usually admitted to the nearest hospital. Thus, sorting of patients to certain kinds of hospitals, e.g., patients of higher socioeconomic status being admitted into better hospitals or patients with more severe conditions are admitted to a better equipped hospital, is less likely. The avoidance of self-selectivity of patients into different kinds of hospitals is important in the current study since separate empirical analyses are carried out for for-profit and not-for-profit hospitals. Moreover, since these four diseases are usually acute and severe, the treatment outcomes of these diseases are relatively straightforward to measure.
We do not include patients hospitalized after March 31, 2003 for two reasons. Firstly, the SARS epidemic, which escalated during the second quarter of 2003 and did not subside until the fourth quarter, represents a shock to the hospital market. Secondly, in 2004 the BNHI introduced the “Hospital Self-Management” and “Hospital Excellence” schemes which allow a participating hospital to have its own expenditure cap. There were slightly less than half of the hospitals participating in the schemes in 2004. The 2003 SARS epidemic and the subsequent changes in the global budget system make it difficult to analyze the global budget system’s impact if our sample period covers these events. Actually, including a relatively narrow time band surrounding the launch of global budgets allows us to avoid unobserved confounding factors.
In our empirical analysis, we examine the impact of global budgeting on a patient’s treatment intensity and outcomes, while controlling for her demographic characteristics and comorbidity conditions. We use the number of points awarded by the BNHI to a hospital for treating a particular patient and patients’ length of stay as proxies for the intensity of treatments. To investigate at what margins hospitals change their treatment intensity, we disaggregate the total number of points into five categories:
-
(a)
Points for medicines,
-
(b)
Points for diagnosis, testing, or screening,
-
(c)
Points for treatment procedures (e.g., surgery),
-
(d)
Points for medical supplies, and
-
(e)
Other points (e.g., room, meals).
We measure a patent’s treatment outcomes based on the incidence of mortality within 30 days after admission. Direct information on patients’ mortality is not available from the NHI database. We infer patients’ mortality from their (a) withdrawal from the NHI and (b) the absence of any claim records of medical care utilization within one year after withdrawal. The four diseases that we study are life-threatening, patients with these diseases will need medical care and surveillance even after being discharged from hospitals. It is not usual for a patient of these diseases to withdraw from NHI shortly after being discharged unless he/she did not survive. Moreover, if it is not because of mortality, it is also not very possible for a patient of such diseases not to seek medical care within one year after hospitalization.
The summary statistics in Table 2 suggest that the four acute diseases’ mortality rate, on average 0.08, is very high. Assuming a point value of NT$1, on average the cost of treating a patient of such diseases in Taiwan is NT$80,731 (i.e., US$2,571.065 at the 2002 exchange rate of 31.4). Moreover, the highest proportion of these medical expenditures is for treatment procedures.
In our empirical analysis, we control for certain regional and patient level characteristics which may affect the outcomes of treatment, e.g., a medical region’s Herfindahl index, and a patient’s gender, age, Charlson Comorbidy Index (denoted CCI score, which is converted to 16 dummies indicating whether a patient’s score is equal to one of the integers in 0-14, or above 14), day of the week dummies, month of the year dummies, disease dummies, dummies indicating whether a patient was admitted to a medical center, a regional hospital or a local hospital, dummies for whether or not a patient had a previous episode of hospitalization for one of the diseases within one year (i.e., new admission). The descriptive statistics of some of these variables are reported in Table 2.
Empirical strategy
To examine the effect of global budgeting on treatment intensity and treatment outcomes we estimate the following fixed effects model.
where \(d \) indexes calendar dates, \(h \) indexes the hospital where patient \(i \) is admitted, \(j \) indexes diseases, and \(g \) indexes regions. The outcome variable \(y_{hid} \) denotes log number of points claimed for different categories of services by hospitals and 30-day mortality. The dummy variable \(\mathtt{GB}_{d}\) is a global budgeting indicator, i.e., \(\mathtt{GB}_{d}=1 \) if \(d \ge \mathrm{July} \ 1, \ 2002 \). Moreover, in (1) \(\mathtt{trend}_{d}\) is a time trend at the daily frequency, \(\varvec{x}_{hid}\) is a vector containing patient characteristics (i.e., CCI scores, age, gender, day of the week and month of the year when admitted, types of disease, and a dummy indicating new-admission patients), \(M_{hid}\) is a dummy variable for medical center, \(H_{hid} \) denotes a region’s Herfindahl index, \(c_{hid} \) and \(r_{hid} \) denote dummy variables for diseases and regions (4 and 6 of them in total), \(\eta _{h}\) is a hospital fixed effect, and \(\epsilon _{hid}\) is a residual; and \(\Big \{\alpha , \varvec{\beta }, \kappa _{jg1}, \kappa _{jg2} , \gamma _1, \gamma _2, \theta _1, \theta _2\Big \} \) are parameters to be estimated. We use \(\eta _{h}\) to control for time-invariant hospital heterogeneity (e.g., accreditation levels, size, location and local demographic characteristics, etc.). The time-invariant unobserved heterogeneity \(\eta _{h}\) is a parameter, which is to be conditioned out, instead of being estimated, in the estimation. Since the characteristics of hospitals do not change very much over time, \(\eta _{h}\) should be sufficient in capturing hospital heterogeneity.
An alternative specification to capture unobserved heterogeneity is the random effects specification, which is equivalent to the random intercept hierarchical model with random intercepts. The random effects specification controls for unobserved heterogeneity by assuming that there is a time-invariant component in the error term and this time-invariant component follows a pre-specified distribution. Features of this distribution are to be estimated in the random effects specification.
Under the random effects specification, it is assumed that the time-invariant error component is uncorrelated with all regressors. If this assumption is violated, the random effects model yields biased estimates for the regressors’ coefficients. By contrast, unobserved heterogeneity \(\eta _h \) is allowed to be correlated with the regressors. If the random error component is uncorrelated with the regressors, the random effects specification yields estimates which are asymptotically equivalent to, but more efficient than, those obtained from the fixed effects specification. See Hsiao (2003) for a comprehensive review.
In addition to its robustness to the possible correlation between the time-invarying unobserved heterogeneity and the regressors, the reason why we choose to adopt the fixed effects specification is that it is especially suitable to the data that we are analyzing: the absence of a rich set of hospital level characteristics. Under the random effects specification, some of the unobserved hospital characteristics, which will become part of the time-invariant error component, are likely to be correlated with the responsiveness of a hospital to the global budget system.
The specification in (1) follows a regression discontinuity design with a parametric specification and calendar day \(\mathtt{trend}_{d} \) as the running variable. Thus, we allow \(y_{hid} \) to follow a quadratic time trend. To make the specification more flexible, we also interact the quadratic time trend with dummies for disease types, hospital accreditation level (i.e., whether a medical center or not), and medical regions. We also interact a region’s Herfindahl index with the quadratic time trend. Under the specification in (1), we identify the effect of global budgeting by detecting a discrete jump or sharp discontinuity in the outcome \(y_{hid} \) surrounding the implementation of global budgeting. This is captured by the coefficient \(\alpha \). The estimation of (1) is via linear regressions with hospital level fixed effects. Our computation of standard errors of the coefficient estimates takes into account clustering at the hospital level.
Nonparametric methods for regression discontinuity designs have been proposed (see Lee and Lemieux 2010). The reason why we adopt a parametric specification in the current study is that we want to control for hospital fixed effects and some other patient characteristics, which are non-negligible determinants of treatment intensity and outcomes. This is infeasible if we use a nonparametric method in terms of computational time. Moreover, the use of a nonparametric method involves the issue of bandwidth choice, which is not trivial.
For the estimation of global budget’s impact on mortality, the fixed effects logit model may be more appropriate in terms of the functional form given that the outcome variable is discrete. However, it is difficult to interpret or quantify the estimation results of a fixed effects logit model. This is because marginal effects cannot be computed using the fixed effects logit model’s estimation results. With the fixed effects being conditioned out and not estimated, we cannot compute the predicted probabilities of the outcome variable, which are needed to compute the marginal effects.
Estimation results
The coefficient estimates of the effects of hospital global budgets on treatment intensity and outcome are summarized in Tables 3 and 4. The estimates for mortality are multiplied by 100 so that they represent percentage points. A more complete set of results is reported in the Appendix. Theories suggest that for-profit hospitals have the strongest incentive to respond to profitable opportunities and this is borne out in the results.
The coefficient estimates of the impact of the launching of global budgets (estimates of \(\alpha \)) in column 3 of Table 3 suggest that there were statistically significant and sizable increases in the number of points claimed by for-profit hospitals for treating cardio-cerebrovascular disease patients. The total number of points claimed increased by 5.3 %, and the number of points for treatment procedures, diagnosis/testing/screening, medicines, and medical supplies increased by 13.3, 5.9, 8.9, and 16.5 %, respectively, while that for “other” medical services did not have a statistically significant change. Moreover, patients’ length-of-stay increased by 4.8 % with the launch of global budgets. These results suggest that acute cardio-cerebrovascular disease patients admitted to for-profit hospitals received substantially more medical services. However, even though there were increases in almost all categories of medical services received by patients in for-profit hospitals, there was no improvement in their treatment outcomes. Actually, their 30-day mortality rate increased slightly by 1.7 %.
Estimates of global budget’s impact for private not-for-profit hospitals are reported in column 2 of Table 3. Private not-for-profit hospitals may have a slightly stronger incentive to respond to financial incentives than government hospitals. There were also substantial increases in the intensity of treatment received by private not-for-profit hospitals’ patients. But these changes are smaller than those of for-profit hospitals. There was a 4.1 % increase in the total number of points claimed, and a 6.9, 5.3, and 5.0 %, respectively, increase in the number of points claimed for treatment procedures, diagnosis/testing/screening, and medicines, while the estimates for changes in points for “other” services and medical supplies are statistically insignificant at conventional levels. Moreover, patients in private not-for-profit hospitals also stayed longer after the launch of global budgets. The length-of-stay increased by 3.8 %. However, the increases in treatment intensity were not translated into better outcomes. We have a statistically insignificant estimate for the effect of global budgets on the 30-day mortality.
Estimates of global budget’s impact for government hospitals are reported in column 1 of Table 3. These estimates suggest that there were no increases in treatment intensity for acute cardio-cerebrovascular disease patients admitted to government hospitals. Actually, there was a 5.3 % decrease in points for “other” medical services. The estimate for global budgets’ impact on the 30-day mortality rate is negative, implying a decrease in mortality rate by 0.86 percentage points, which is statistically insignificant at conventional levels though.
A more complete set of results is reported in the Appendix. While a thorough discussion of these results is out of the scope of the current study and lengthens the paper considerably, we provide a brief discussion below and focus on those for the total number of points. The coefficient estimates for disease types indicate that compared with hemorrhagic stroke patients, those suffering from AMI, Ischemic heart disease and ischemic stroke received a larger quantity of medical care in government and private not-for-profit hospitals. However, the coefficient estimates are statistically significant for private not-for-profit hospitals. The relevant coefficient estimates are statistically insignificant for for-profit hospitals. These coefficient estimates probably reflect differences in the costs of treating different types of patients.
The coefficient estimates for new patients suggest that new patients of ischemic stroke receive less medical care in all types of hospitals, while those suffering from ischemic heart disease and hemorrhagic stroke receive less medical care only in government and private not-for-profit hospitals and receive more in for-profit hospitals (the coefficient estimate for new patients of ischemic heart disease is statistically insignificant though). New AMI patients receive more medical care in all types of hospitals, albeit the coefficient estimate is statistically insignificant for for-profit hospitals.
While patients’ age seems not to affect the amount of medical care they receive, male patients receive more in all types of hospitals. This reflects the phenomenon that male patients’ conditions are usually more severe. The coefficient estimates for the days of the week (at admission) dummies are mostly insignificant, except those for “Monday” (negative) and “Sunday” (positive) in for-profit hospital and “Thursday” (positive) and “Saturday” (positive) for government hospitals compared with “Wednesday” (the reference group) for the relevant type of hospitals. The patterns of the days of the week coefficients seem to be consistent with the weekend effects found in the literature: patients admitted on weekends (Saturday or Sunday) receive more medical care probably because hospitals are insufficient staffed on weekends.
The above discussion indicates that there are a lot of differences in the coefficients for different types of hospitals, especially those between for-profit hospitals and the other two types of hospitals. The differences in the coefficient estimates suggest that there is a lot of heterogeneity in the behavior of government, private not-for-profit and for-profit hospitals, probably arising from differences in financial incentives, and hospital equipment and scale.
To summarize, our estimation results suggest that, as predicted by theories, the quantity of treatments received by patients in for-profit and private not-for-profit hospitals increased with the implementation of global budgeting, while that for government hospitals remained unchanged. The increases in treatment intensity are larger for for-profit hospitals. However, the treatment outcome, measured by 30-day mortality, did not improve in for-profit and private not-for-profit hospitals. We have also examined the mortality rates of other horizons (e.g., 7- and 90-day) and obtained similar results, which are available upon request. Given that the increase in medical care utilization did not led to an improvement in treatment outcomes, our estimation results seems to indicate a misallocation or waste of medical resources.
Discussion
In this section, we discuss how our results are related to those obtain by previous studies. This is followed by results of robustness checks on our estimates. Finally, we discuss the implications of several changes to the payment scheme of Taiwan’s NHI on this study’s empirical analysis.
Our results that global budgets led to an increase in medical care utilization are consistent with those obtained by previous empirical studies for Canada (Rochaix 1993, and Hurley et al. 1997) and Taiwan (Lee and Jones 2004; Chen et al. 2007, and Cheng et al. 2009). However, our finding that the increase in medical care utilization did not result in better outcomes are in contrast with those obtained by Chang et al. (2011) and Tung and Chang (2010). The differences may be due to the fact that there were several adjustments to the NHI payment scheme during their sample period, covering 1997–2008, while most of these adjustments were avoided in our much shorter sample period of January 2001–March 2003.
Moreover, our empirical results are consistent with the predictions of Fan’s et al. (1997) under the scenario where providers do not coordinate and Benstetter and Wambach (2006) under the low price equilibrium. On the contrary, Mougeot and Naegelen’s (2005) prediction of a lower medical care quantity under the assumption that providers choose the level of service quality and cost-minimization effort to maximize profit is refuted.
For the purpose of robustness check, we estimated model (1) based on a sample excluding patients staying in hospital for more than 65 days, or younger than 35 or older than 80. Patients in this restricted sample is less heterogeneous than those in the full sample. Table 4 summarizes the results. Qualitatively, the results are similar to that in Table 3 for the full sample: there was an increase in the treatment intensity but no improvement in the outcome for patients in for-profit hospitals.
In addition, we have estimated a hierarchical model with a random intercept and a random coefficient for the effect for global budgets. The results based on the hierarchical model, available upon request, are qualitatively (i.e., in terms of the existence and direction of effects) very similar to those obtained with the fixed effects specification.
There were several minor changes in the payment system that were effective surrounding the timing of the implementation of global budgets. However, as explained below, these changes are not likely to affect our empirical analysis. Firstly, BNHI introduced a case payment system to several standardized treatment items on July 1, 1999. However, the number of items covered by this case payment system was limited. Also, there was an increase in the payment levels for some treatment items starting from June 1, 2001. However, the extent of the change was small in magnitude (0.62–4.8 % rise in the payment levels) and the items covered were limited. Furthermore, since the raise was applied (effective June 1, 2001) one year before the implementation of global budgets, it is unlikely to affect our identification of global budget’s effect.
Secondly, BNHI increased the copayment for outpatient care significantly in 2002/9. However, since the observations in our sample were hospitalized patients with AMI, ischemic heart diseases and stroke, it is unlikely that an increase in the copayment of outpatient care would also increase the likelihood, frequency or quantities of inpatient care for substitution reasons. After all, the admission of a patient to the inpatient department is determined by a doctor, not by the patient. Another reason why this change would not confound our results is that, in absolute terms, the increases (from around US$5 to US$7 and US$3.3 to US$4.7, respectively for medical centers and regional hospitals) were small and they were unlikely to trigger any inpatient-outpatient service substitution by acute disease patients. Therefore, we believe that the increase in the copayment of outpatient care would not confound our estimation of the effect of global budgeting.
Conclusion
This study investigates the impact of hospital global budgeting on treatment intensity and outcomes of AMI, ischemic heart disease, hemorrhagic stroke, and ischemic stroke patients. We look at the case of Taiwan, which launched hospital global budgets in 2002.
Previous studies’ theoretical results suggest that medical service providers are likely to increase their quantity of service supplied. Economic theories also predict that for-profit hospitals have the highest degree of responsiveness to profitable opportunities and government hospitals the least, implying the former are the most responsive to global budgets and the latter the least.
We perform our empirical analysis for government, private not-for-profit, and for-profit hospitals separately and look at the differences in their treatment intensity and the outcome’s response to global budgets. Our empirical results suggest that there were sizable increases in for-profit hospitals’ treatment intensity, especially in terms of the number of points claimed for treatment procedures, diagnosis/testing/screening, medicines and medical supplies, and patients’ length-of-stay. However, our results show no improvement in treatment outcome for patients in for-profit hospitals in terms of the 30-day mortality rate after the launch of hospital global budgets. We have also examined the mortality rates of other horizons (e.g., 7- and 90-day) and obtained similar results, which are available upon request.
The treatment intensity of private not-for-profit hospitals increased moderately with the launch of global budgets. There were no changes in treatment outcomes for patients admitted to these hospitals. By contrast, government hospitals did not increase their treatment intensity at all. There was no change in their treatment outcomes either. The differences in the three types of hospitals’ changes in treatment intensity are in accord with theories on government and not-for-profit organizations’ behavior. The increases in for-profit and private not-for-profit hospitals’ treatment intensity are also consistent with theoretical results of previous studies.
Our results indicate that the increases in medical services devoted to treatment may represent a misallocation or waste of resources because treatment outcomes did not improve. This implies that aggregate expenditure caps should be supplemented by other designs to prevent resources misallocation. For example, Benstetter and Wambach’s (2006) suggestion of setting a minimum price for medical services may alleviate the excess use of medical resources. Alternatively, on top of global budgets, a DRG-based payment system instead of a medical procedure-based fee-for-service payment system may prevent hospitals from providing unnecessary medical services to patients. Furthermore, setting individual expenditure caps for hospitals, similar to Taiwan’s “Hospital Excellence” scheme, introduced in 2004, may mitigate the “common property” problem caused by global budgets. But this involves high administrative costs. We leave to future research to find out the exact effects of these measures in a global budget system.
Notes
References
Benstetter, F., & Wambach, A. (2006). The treadmill effect in a fixed budget system. Journal of Health Economics, 25, 146–169.
Chang, G.-M., Cheng, S.-H., & Tung, Y.-C. (2011). Impact of cuts in reimbursement on outcome of acute myocardial infarction and use of percutaneous coronary intervention: a nationwide population-based study over the period 1997 to 2008. Medical Care, 49(12), 1054–1061.
Chen, F. J., Laditka, J. N., Laditka, S. B., & Xirasagar, S. (2007). Providers’ response to global budgeting in Taiwan: What were the initial effects? Health Service Management Research, 20, 113–120.
Cheng, S.-H., Chen, C.-C., & Chang, W.-L. (2009). Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy, 92(2–3), 158–164.
Cheng, S.-H., Chen, C.-C., & Tsai, S.-L. (2012). The impacts of DRG-based payments on health care provider behaviors under a universal coverage system: A population-based study. Health Policy, 107(2–3), 202–208.
Christianson, J. B., & Conrad, D. (2011). Provider payment and incentives. In S. Glied & P. C. Smith (Eds.), The Oxford handbook of health economics. Oxford: Oxford University Press.
Cutler, D. M. (1995). The incidence of adverse medical outcomes under prospective payment. Econometrica, 63(1), 29–50.
Dafny, L. S. (2005). How do hospitals respond to price changes? The American Economic Review, 95, 1525–1547.
Department of Health. (2003a). Statistics of Causes of Death, 2002. Republic of China (Taiwan): Executive Yuan.
Department of Health. (2003b). Health Statistics in Taiwan, 2002. Republic of China (Taiwan): Executive Yuan.
Docteur, E., & Oxley, H. (2004). Health-system reform: Lessons from experience. In Towards High-Performing Health Systems. OECD Policy Studies, Paris: Organization for Economic Co-Operation and Development.
Duggan, M. G. (2000). Ownership and public medical spending. Quarterly Journal of Economics, 115, 1343–1373.
Fan, C. P., Chen, K. P., & Kan, K. (1998). The design of payment systems for physicians under global budget—an experimental study. Journal of Economic Behavior and Organization, 34(2), 295–311.
Eggleston, K., Shen, Y.-C., Lau, J., Schmid, C. H., & Chan, J. (2008). Hospital Ownership and quality of care: What explains the different results in the literature? Health Economics, 17, 1345–1362.
Hansmann, H. (1980). The role of nonprofit enterprise. Yale Law Journal, 89, 835–901.
Hsiao, C. (2003). Analysis of panel data (2nd ed.). Cambridge: Cambridge University Press.
Horwitz, J. R. (2005). Making profits and providing care: Comparing nonprofit, for-profit, and government hospitals. Health Affairs, 24, 790–801.
Horwitz, J., & Nichols, A. (2009). Hospital ownership and medical services: Market mix, spillover effects and nonprofit objectives. Journal of Health Economics, 28, 924–937.
Hurley, J., Lomas, J., & Goldsmith, L. J. (1997). Physician responses to global physician expenditure budgets in Canada: A common property perspective. The Milbank Quarterly, 75(3), 343–364.
Kornai, J. (1986). The soft budget constraint. Kyklos, 39, 3–30.
Kornai, J. (2009). The soft budget constraint syndrome in the hospital sector. International Journal of Health Care Finance and Economics, 9, 117–135.
Kornai, J., Maskin, E., & Roland, G. (2003). Understanding the soft budget constraint. Journal of Economic Literature, 41, 1095–1136.
Le Grand, J. (2003). Methods of cost containment: Some lessons from Europe. Working Paper, London School of Economics.
Lee, D. S., & Lemieux, T. (2010). Regression discontinuity designs in economics. Journal of Economic Literature, 48, 281–355.
Lee, M. C., & Jones, A. M. (2004). How did dentists respond to the introduction of global budgets in Taiwan? An evaluation using individual panel data. International Journal of Health Care Finance and Economics, 4, 307–326.
Lien, H.-M., Chou, S.-Y., & Liu, J.-T. (2008). Hospital ownership and performance: Evidence from stroke and cardiac treatment in Taiwan. Journal of Health Economics, 27(5), 1208–1223.
Louis, D. Z., Yuen, E. J., Braga, M., Cicchetti, A., Rabinowitz, C., Laine, C., & Gonnella, J. S. (1999). Impact of a DRG-based hospital financing system on quality and outcomes of care in Italy. Health Service Research, 34(1 Part 2), 405–415.
McClellan, M. B., & Staiger, D. O. (2000). Comparing hospital quality at for-profit and not-for-profit hospitals Chapter 3. In D. M. Cutler (Ed.), The changing hospital industry: Comparing for-profit and not-for-profit institutions (pp. 93–112). Chicago: University of Chicago Press.
Miller, H. D. (2009). From volume to value: Better ways to pay for health care. Health Affairs, 28(5), 1418–1428.
Mougeot, M., & Naegelen, F. (2005). Hospital price regulation and expenditure cap policy. Journal of Health Economics, 24, 55–72.
Rogers, W. H., Draper, D., Kahn, K. L., Keeler, E. B., Rubenstein, L. V., Kosecoff, J., et al. (1990). Quality of care before and after implementation of the DRG-based prospective payment system: A summary of effects. Journal of American Medical Association, 264(15), 1989–1994.
Rochaix, L. (1993). Financial incentives for physicians: the Quebec experience. Health Economics, 2, 163–176.
Silverman, E., & Skinner, J. (2004). Medicare upcoding and hospital ownership. Journal of Health Economics, 23, 369–389.
Shen, Y.-C., & Eggleston, K. (2009). The effect of soft budget constraints on access and quality in hospital care. International Journal of Health Care Finance and Economics, 9, 211–232.
Sloan, F. A. (2000). Not-for-profit ownership and hospital behavior. In: Culyer, A. J., Newhouse, J. P. (Eds.) Handbook of Health Economics, Vol. 1, Part B (pp. 1141–1174). Elsevier.
Sloan, F. A., Picone, G. A., Taylor, D. H, Jr, & Chou, S.-Y. (2001). Hospital ownership and cost and quality of care: Is there a dime’s worth of difference? Journal of Health Economics, 20, 1–21.
Tung, Y.-C., & Chang, G.-M. (2010). The effect of cuts in reimbursement on stroke outcome: A nationwide population-based study during the period 1998 to 2007. Stroke, 41(3), 504–509.
Weisbrod, B. (1977). Voluntary nonprofit sector. Lexington, Mass: DC Heath.
Wilson, J. (1989). Bureaucracy. Washington, D.C.: Basic Books.
Wolfe, P. R., & Moran, D. W. (1993). Global budgeting in the OECD countries. Health Care Financing Review, 14(3), 55–76.
Acknowledgments
The authors are grateful to the financial supports from the Ministry of Science Technology (NSC97-2401-H-008-013-MY3).
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Tables 5, 6, 7, 8, 9, 10, 11 and 12.
Rights and permissions
About this article
Cite this article
Kan, K., Li, SF. & Tsai, WD. The impact of global budgeting on treatment intensity and outcomes. Int J Health Care Finance Econ 14, 311–337 (2014). https://doi.org/10.1007/s10754-014-9150-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-014-9150-0