Abstract
Aims/hypothesis
To estimate the prevalence and incidence of diabetes mellitus and impaired glucose regulation (IGR) in a Chinese population aged 20–94 years.
Subjects and methods
A group of 5,628 randomly selected adults, aged 20–94 years, living in the Huayang and Caoyang communities in Shanghai, China, were investigated between 1998 and 2001. During 2002-04, 2,666 subjects were followed up. All the participants underwent anthropometric measurements, blood biochemical analyses and a 75-g OGTT.
Results
Based on the 2000 census data of China, the age-standardised prevalences were 6.87% for diabetes and 8.53% for IGR at baseline. More than two in five cases with diabetes were undiagnosed. The age-adjusted prevalence of diabetes and IGR increased with age. The age-adjusted prevalences of hypertension, dyslipidaemia and overweight in males were significantly higher (p < 0.001) than in females. The 3-year cumulative incidence rates of diabetes and IGR were 4.96 and 11.10%, respectively. The relative risk of developing diabetes was significantly higher in subjects with IGR than in subjects with NGT (p < 0.001).
Conclusions/interpretation
The prevalence and incidence rates for diabetes or IGR have increased dramatically over the last decades, especially in younger age groups. A large proportion of cases are undiagnosed. We strongly recommend that population-based diabetes screening programmes should be implemented and generalised for younger people.
Similar content being viewed by others
Introduction
Diabetes mellitus is one of the most challenging public health problems throughout the world and has increased at an alarming rate over the past few decades. In the early 1980s, a national survey based a population exceeding 300,000 in 14 Chinese provinces revealed that the total standardised prevalence of diabetes was 6.74 per thousand. As part of the research, the prevalence of diabetes in Shanghai was 5.88 per thousand and the prevalence among young people aged 20–29 years was fairly low, no more than 1 in 1,000. As a modern city, the lifestyle and the inhabitant environment in Shanghai have changed dramatically over the past 20 years. For example, overnutrition or dietary imbalance, long-term sedentary occupations and lack of physical activity all contribute to the incidence of chronic diseases, such as diabetes, cardiovascular events, and so on, especially in city dwellers. This survey aims to provide detailed information on the prevalence and incidence of diabetes and impaired glucose regulation (IGR) in a Chinese urban population at the turn of the century.
Subjects and methods
Subjects
The target population included residents over 20 years of age who had been living in Shanghai for more than 10 years. Shanghai is a cosmopolitan city with a population of more than 16 million. The present study was a cross-sectional survey based on two nearby urban communities, with random sampling. Since 1996, The Shanghai Diabetes Institute has conducted a series of genetic and clinical epidemiological studies (Shanghai Diabetes Studies) of diabetes and associated metabolic disorders in Shanghai. The Huayang and Caoyang communities, two middle-income communities in Shanghai, were selected for the survey. From these communities, 5,994 individuals aged >15 years were enrolled from September 1998 to May 2000 (Huayang) and from July 2001 to November 2001 (Caoyang). Informed consent was obtained from each participant before the survey. A total of 5,628 subjects aged from 20 to 94 years were selected and examined. Individuals who suffered from cancer, severe disability or severe psychiatric disturbance were excluded.
During 2002-04, 2,666 non-diabetic participants had a second blood glucose analysis in a 3-year follow-up study. Follow-ups were carried out when it had been 3 years since the original examination. The protocol was in accordance with The Helsinki Declaration and was approved by the local ethical committee. The investigation team consisted of a diabetic specialist, a physician, an epidemiologist, a nurse, staff from the local health centre, and the monitors. The team members were trained prior to the survey. Data entries were made in duplicates by key-punchers and verified correct.
Methods
Participants arrived at the local hospital at 06.00–07.00 hours following an overnight fast. A self-administered questionnaire, which contained questions about the subject’s medical history, smoking habits, alcohol intake, diet, physical activity and occupation, was completed in advance. The anthropometric indices of height and weight were measured while the participants were barefoot and in light clothing. BMI was calculated as weight divided by height squared (kg/m2). Waist circumference (WC) and hip circumferences were measured in duplicate with the subjects standing relaxed and in underwear only and averaged out. WC was measured at the point between the costal margin and iliac crests which yielded the minimum measurement. Hip circumference was measured around the buttocks at the level that yielded the maximum measurement. The WHR was calculated as the ratio of the WC to the hip circumference. Femoral circumference was measured at the midpoint between the iliac crest and the upper margin of the patella. Blood pressure measurements were taken three times using a sphygmomanometer and then averaged.
After a fasting venous blood sample was collected, each participant received a 75-g OGTT, except for those with a validated history of diabetes mellitus. Plasma glucose levels were measured using the glucose oxidase method. Serum true insulin was assayed used a bio-antibody technique (Linco, St Louis, MO, USA). Serum lipid profiles, including measurements of total cholesterol, triacylglycerol, HDL-cholesterol and LDL-cholesterol, were also obtained with an automated biochemical instrument by RIA based on the double-antibody technique (DPC, Los Angeles, CA, USA). All control values were consistent with the standard recommended by the Shanghai Clinical Testing Center.
The diagnostic standards for diabetes and its complications were as follows. Diabetes and IGR were diagnosed according to the standard set by the American Diabetes Association (ADA) in 1997. IGR is defined as IFG (fasting plasma glucose [FPG] ≥ 6.1 mmol/l and <7.0 mmol/l, 2-h postprandial plasma glucose [2hPG] < 7.8 mmol/l) and/or IGT (FPG ≥ 6.1 mmol/l, 2hPG ≥ 7.8 mmol/l and <11.1 mmol/l). Thus it can be classified into three types as isolated IFG (FPG ≥ 6.1 mmol/l and <7.0 mmol/l, 2hPG < 7.8 mmol/l), isolated IGT (FPG ≥ 6.1 mmol/l, 2hPG ≥ 7.8 mmol/l and <11.1 mmol/l), and combined IGT (FPG ≥ 6.1 mmol/l and <7.0 mmol/l, 2hPG ≥ 7.8 mmol/l and <11.1 mmol/l). The criteria for hypertension issued by WHO in 1999 (systolic blood pressure of 140 mmHg and/or diastolic blood pressure of 90 mmHg) were used. Dyslipidaemia was diagnosed according to the American National Cholesterol Education Program (Adult Treatment Panel III). The diagnosis criteria for obesity and overweight issued by WHO in 1997 were used.
Statistical analysis
Statistical analyses were performed using SAS statistical software. Descriptive data are given as means ± SD. One-way ANOVA was applied to compare differences of continuous variables between subgroups. Relative risk (RR) was calculated by using the Mantel–Haenszel chi-square test. Age-standardised estimates of prevalence were calculated by the direct method, where the 2000 census of the Chinese adult population aged 20–94 years was taken as the standard. A p value of <0.05 was considered statistically significant.
Results
Prevalence of diabetes and IGR
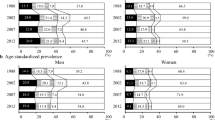
As shown in Table 1, the crude prevalence estimates of diabetes and IGR in this survey were 11.35 and 11.74%, respectively. After age and sex standardisation based on the 2000 China census data, the prevalences were 6.87% (7.35% for men and 6.36% for women) for diabetes and 8.53% for IGR (9.60% for men and 7.43% for women). Of the 639 patients with diabetes, 56.8% (n = 363) had been previously diagnosed as diabetic. The proportion of newly diagnosed diabetes (n = 276) accounted for 4.90% of the total participants. Prevalence of diabetes increased with age, from 0.33% in the 20- to 29-year age group to 20.55% in the 80-year and older age group. Before the age of 50 years, the prevalence of diabetes was <10% in both males and females. In most of the age groups, men had a significantly higher prevalence of diabetes than women. However, the prevalence of diabetes in females over the age of 70 was higher than that in males. The prevalence of IGR also increased with age. Before middle age, the prevalence of IGR in women was significantly lower than that in men, while between the ages of 60 and 79 years, the prevalence of IGR in women was significantly higher than that in men. The crude rates of isolated IFG, isolated IGT and combined IGT were 8.69, 6.56 and 3.48%, respectively, whereas this was not seen in isolated IFG and combined IGT. The crude rate of isolated IGT showed an increase with age (p < 0.01) for both men and women (Fig. 1).
Stratified by various subgroups of BMI (Fig. 2), the crude rate of diabetes and IGR both had a significant positive correlation with BMI, in both men (p < 0.05) and women (p = 0.001). Stratified by various subgroups of WC, the crude rate of diabetes had a significant positive correlation with BMI in both males (p = 0.002) and females (p = 0.013). The crude rate of IGR in male increased with the increment of WC but was not significantly linear (p = 0.080). In normal-weight and normal-WC subgroups, the crude rates of diabetes and IGR were higher in men than in women, while with the increment of BMI and WC, the crude rates of diabetes and IGR in females were close to those in men, or even exceeded those in men. The crude rates of diabetes and IGR in females with BMIs ranging from 23 to 25 kg/m2 were 11.0 and 11.6%, respectively, which are double those of females of normal weight (p < 0.01). The same increment existed in the female subgroups with WC ranging from 0.80 to 0.85 m compared with those with normal WC.
Crude rates of diabetes and IGR in various subgroups of BMI (a, b) and (c, d), respectively. White bar, men; black bar, women. a r = 0.969, p = 0.013 for men, r = 0.999, p = 0.001 for women. b r = 0.062, p = 0.0038 for man, r = 0.999, p = 0.001 for women. c r = 0.998, p = 0.002 for men, r = 0.987, p = 0.013 for women. d r = 0.920, p = 0.080 for men, r = 0.009, p = 0.002 for women
Incidence of diabetes and IGR
Three years after the original survey, 2,666 non-diabetic subjects, approximately 53.44% of the original non-diabetic subjects, were followed up. There were no significant differences in age, sex or BMI between returnees and non-returnees. Among the other 2,323 non-diabetic subjects, 105 individuals had died and the rest had migrated such that we could not contact them. A total of 2,608 subjects (97.82%) received an OGTT and the other 58 subjects had their FPG measured. As the values of FPG of 43 subjects without a 2hPG measurement were <7.0 mmol/l, they were excluded from analysis. The follow-up study revealed that 1.99% of the subjects with NGT had developed diabetes, whereas 23.42% of subjects with IGR developed diabetes. The combined IGT showed the highest propensity for diabetes (Table 2). The RR of developing diabetes was significantly higher in subjects with IGR than in subjects with NGT (p < 0.001). The annual incidence of diabetes in subjects with NGT and IGR was 0.66 and 7.81%, respectively. The annual incidence of diabetes and IGR was 1.65 and 3.70%, respectively. After 3 years, the cumulative incidence of diabetes and IGR was 4.96 and 11.10%, respectively. The cumulative incidences of developing isolated IFG, isolated IGT and combined IGT in this population after 3 years were 1.46, 8.76 and 0.88%. In IGR subjects with FPG ranging from 6.1 to 6.9 mmol/l, combined with or without postprandial hyperglycaemia, the RR of future diabetes was significantly higher than in NGT subjects with FPG < 5.6 mmol/l (p < 0.001). Even in NGT subjects with FPG ranging from 5.6 to 6.0 mmol/l, the RR of developing diabetes was significantly higher than those of NGT subjects with FPG < 5.6 mmol/l (p < 0.001), especially those combined with postprandial hyperglycaemia.
Prevalence of associated metabolic disorders
Overall, 38.61% of the participants exhibited hypertension, 40.33% demonstrated dyslipidaemia, 29.95% were overweight and 4.53% were obese. After age standardisation, the overall prevalences of hypertension, dyslipidaemia, overweight and obesity were 26.36, 35.04, 25.55 and 4.02%, respectively. The male population had a higher prevalence of hypertension, dyslipidaemia and overweight than the female (p < 0.001), whereas women were more obese than men (p < 0.001) (data not shown).
Sex differences in clinical characteristics among various glucose tolerance populations
As shown in Table 3, in normal-blood-glucose subjects, age, WC, WHR, systolic pressure, diastolic pressure and triacylglycerol were significantly higher in men than in women, whereas FPG, 2hPG, total cholesterol, HDL-cholesterol and LDL-cholesterol were significantly lower in men than in women. In both IGR and diabetic subjects, BMI, total cholesterol, HDL-cholesterol and LDL-cholesterol were significantly higher in women than in men, whereas WHR was significantly lower in women than in men.
Discussion
The prevalence of type 2 diabetes and IGT was reported to be about 1% for each sex among a sample of 110,660 men and women aged 25–74 years, who were living in an urban Chinese community in 1986 [1, 2]. The 1994 China National Diabetes Survey examined 224,251 men and women aged 25–64 years, and estimated that the prevalence of diabetes and IGT was 2.5 and 3.2%, respectively [3]. The International Collaborative Study of Cardiovascular Disease in Asia [4], which was conducted from 2000 to 2001, included a nationally representative sample of 15,540 adults, aged 35–74 years. This study revealed that the prevalence of self-reported diagnosed diabetes was 1.3%, of undiagnosed diabetes 4.2%, and of IFG 7.3% in Chinese adults. Another publication of epidemiological research [5] in China indicated that the prevalence of undiagnosed diabetes was high in both rural and urban areas, yet the proportion of undiagnosed cases among diabetic subjects was significantly higher in rural than in urban areas, which indicated the lack of public awareness and shortage of medical facilities.
The present study surveyed the urban population aged from 20–94 years, living in Shanghai, the east coastal area of China. Although the prevalence of diabetes in China estimated in this study (6.87%) is lower than those reported for other countries or regions in East Asia, which reflects differences in environmental influences as well as in genetic susceptibility (9.0% in Taiwan, 1996 [6]; 8.1% in Singapore, 1998 [7]; and 9.8% in Hong Kong, 1995–1996 [8]), it was somewhat higher than the data of 1994 in China [3], especially in young people (0.86% [aged 20–39 years] vs 0.30% [aged 25–34 years]). In addition, the age-standardised prevalence of diabetes estimated in the present study was higher than that in rural areas [4, 5]. This is because of urbanisation-associated unhealthy diet, sedentary lifestyle and obesity. Comparing the two Chinese nutrition surveys in 1982 and 1992, the standard of living and the composition of the diet changed remarkably. The prevalence of obesity in younger groups aged 20–29 years in 1998 [9] (3.77%) had already exceeded the overall prevalence of overweight/obesity in 1982 and 1992, which was <3%. An analysis in Shanghai revealed that the expenditure on corn after 1980 declined 22% compared with that in 1952, while that on animal food increased fivefold. Such unhealthy dietary composition, with high fat, high cholesterol and low carbohydrate levels, directly or indirectly induced the disorders of metabolism of glucose and lipid which result in incident diabetes. Similar to other research, the prevalence of diabetes and IGR increased with age in both male and female populations. Nearly 50% of the diabetic subjects in the present study had no awareness of their illness. Thus, the high incidence of diabetes and IGR in Chinese adults suggested an urgent need to establish a national education programme in China to promote regular community and clinic-based diabetes screening for early detection of diabetes and IGR, and screening the target population aged 20–39 years should be emphasised.
The reduction of the cut-off point of FPG from 6.1 to 5.6 recommended by ADA in 2003 has been widely debated, especially in those publications dealing with its merits in predicting future diabetes [10–13]. In the present study, we found a significantly higher risk of developing diabetes in non-diabetic subjects with FPG ranging from 5.6 to 6.0 mmol/l, compared with NGT subjects with FPG <5.6 mmol/l. Thus we recommend that a 75-g OGTT and a follow-up study should be applied to a person when his or her FPG is in the range of 5.6 to 6.0 mmol/l.
During middle age (50∼69 years), the prevalence of diabetes in males was higher than that of females, whereas after the age of 70, it was quite the opposite. A similar situation was also reported in India and Oman [14, 15]. Also males had a propensity for hypertension, dyslipidaemia and overweight, whereas females were more obese and exhibited much higher BMIs and higher levels of total cholesterol and LDL-cholesterol than males, especially in those with abnormal glucose tolerance. One possible explanation for such a male preponderance in early middle age may be that males are more susceptible to the consequences of indolence and obesity, possibly due to differences in insulin sensitivity and regional fat deposition [16]. Possible due to the longer life-span of women, such a male preponderance disappeared in older age groups.
In summary, the prevalence of diabetes and IGR in a Chinese urban population has increased at a dramatic rate over the past decades. The onset of type 2 diabetes begins at younger ages than previously expected. More than two out of every five people with diabetes are undiagnosed. This finding is indicative of a lack of population-based diabetes screening programmes and a recent and relatively rapid increase in the incidence of diabetes. Our results should encourage the development and implementation of such a screening programme in order to minimise the medical and financial costs of diabetes-related complications.
Abbreviations
- 2hPG:
-
2-h postprandial plasma glucose
- ADA:
-
American Diabetes Association
- FPG:
-
fasting plasma glucose
- IGR:
-
impaired glucose regulation
- RR:
-
relative risk
- WC:
-
waist circumference
References
Li GW, Hu YH, Pan XR (1996) Prevalence and incidence of NIDDM in Daqing City. Chin Med J (Engl) 109:599–602
Pan XR, Hu YH, Li GW et al (1993) Impaired glucose tolerance and its relationship to ECG-indicated coronary heart disease and risk factors among Chinese. Diabetes Care 16:150–156
Pan XR, Yang WY, Li GW, Liu J (1997) Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care 20:1664–1669
Gu D, Reynolds K, Duan X et al (2003) Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia (InterASIA). Diabetologia 6:1190–1198
Dong Y, Gao W, Nan H et al (2005) Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabet Med 22:1427–1433
Lu FH, Yang YC, Wu JS, Wu CH, Chang CJ (1998) A population-based study of the prevalence and associated factors of diabetes mellitus in southern Taiwan. Diabet Med 15:564–572
Cutter J, Tan BY, Chew SK (2001) Levels of cardiovascular disease risk factors in Singapore following a national intervention program. Bull World Health Organ 79:908–915
Janus ED, Watt NM, Lam KSL et al (2000) The prevalence of diabetes, association with cardiovascular risk factors and implications of diagnostic criteria (ADA 1997 and WHO 1998) in a 1996 community-based population study in Hong Kong Chinese. Diabet Med 17:741–745
Jia WP, Xiang KS, Chen L, Lu JX, Wu YM (2002) Epidemiological study on obesity and its comorbidities in urban Chinese older than 20 years of age in Shanghai, China. Obes Rev 3:157–165
Cicero AF, Dormi A, Nascetti S et al (2005) Relative role of major risk factors for type 2 diabetes development in the historical cohort of the Brisighella Heart Study: an 8-year follow-up. Diabet Med 22:1263–1266
Shaw JE, Zimmet PZ, Hodge AM et al (2000) Impaired fasting glucose: how low should it go? Diabetes Care 23:34–39
Gabir MM, Hanson RL, Dabelea D et al (2000) The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care 23:1108–1112
Tirosh A, Shai I, Tekes-Manova D et al (2005) Normal fasting plasma glucose levels and type 2 diabetes in young men. N Engl J Med 353:1454–1462
Ramachandran A, Snehalatha C, Kapur A et al (2001) High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 44:1094–1101
Al-Lawati, Al Riyami M, Mohammed AJ, Jousilahti P (2002) Increasing prevalence of diabetes mellitus in Oman. Diabet Med 19:954–957
Gale EAM, Gillespie KM (2001) Diabetes and gender. Diabetologia 44:3–15
Acknowledgements
This study was supported by the Key Project of Shanghai, China (04DZ9501 and 01ZD0021).
Duality of interest
All the authors declare no duality of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jia, W.P., Pang, C., Chen, L. et al. Epidemiological characteristics of diabetes mellitus and impaired glucose regulation in a Chinese adult population: the Shanghai Diabetes Studies, a cross-sectional 3-year follow-up study in Shanghai urban communities. Diabetologia 50, 286–292 (2007). https://doi.org/10.1007/s00125-006-0503-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-006-0503-1