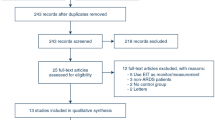
Abstract
Objective
To determine the effects of body and head positions on the spatial distribution of ventilation in nonintubated spontaneously breathing and mechanically ventilated infants using electrical impedance tomography (EIT).
Design and setting
Prospective study in a neonatal intensive care unit.
Patients
Ten spontaneously breathing (gestational age 38 weeks, postnatal age 13 days) and ten mechanically ventilated infants (gestational age 35 weeks, postnatal age 58 days).
Interventions
Supine and prone postures with different head positions (midline and rotated to the left and right side).
Measurements and results
The distribution of ventilation in the chest cross-section was repeatedly determined from EIT data in each body/head position studied. During spontaneous breathing the tidal volumes in the left lung region were reduced in the supine posture with the head turned to the left as well as in the prone posture with the head rotated to either side when compared with the supine posture with the head in the midline position. During mechanical ventilation the tidal volumes in the left lung region were unaffected by the body and head position except for the prone posture combined with the leftward head rotation which reduced them. In both types of ventilation the tidal volumes in the right lung region were unaffected by the change in body/head position.
Conclusion
The results indicate that the spatial distribution of ventilation is influenced by the body and head position in spontaneously breathing infants. Prone posture with the leftward head rotation has the most prominent effect which is detectable even during mechanical ventilation.
Similar content being viewed by others
Introduction
Little is currently known about the regional characteristics of lung ventilation in preterm and term neonates. The effects of anatomical and physiological factors on regional lung ventilation in this age group are difficult to study. Computed or magnetic resonance tomography, which is well established in studies on adult subjects, cannot be used in small infants. Plain chest radiography can only be used for diagnosis, and therefore radiographs are available only for infants suffering from lung disease or undergoing artificial ventilation therapy. Moreover, chest radiographic examinations are not able to assess the functional aspects of regional lung ventilation. The only method available to indirectly study regional lung ventilation in small infants free of lung disease is the inert gas washout technique [1, 2, 3]. This technique which requires the use of an endotracheal tube or a face mask can detect inhomogeneities in lung ventilation but cannot exactly locate them. Consequently there are few studies of unsedated spontaneously breathing infants with natural, unmodified respiratory mechanics.
In recent years electrical impedance tomography (EIT) has been identified as a possible new tool for studying regional lung function in experimental and clinical studies [4, 5, 6, 7]. Its ability to determine regional lung volume changes has been validated [8, 9, 10, 11]. EIT uses a radiation-free measuring principle and allows examinations to be performed during long periods of time at scan rates up to about 40 scans per second. These characteristics make EIT attractive for monitoring applications in a clinical setting, particularly in intensive care patients [12, 13, 14].
We used EIT in a study of spontaneously breathing preterm and term neonates shortly before their discharge from the neonatal intensive care unit (NICU) [15]. We studied the effect of three different postures on the distribution of lung ventilation in the chest cross-section during rapid tidal breathing and sighs. The study revealed one unexpected finding: the prone position increased the asymmetry of the distribution of inspired air between the right and left lungs during tidal breathing by lowering the ventilation in the left lung region.
There are a few indications that the head position may influence respiratory mechanics in very small infants [16], and that it may have important clinical implications [17]. The effect of head position was not followed in our previous study, and its possible role in generating the asymmetric ventilation distribution during spontaneous breathing in the prone position could thus be neither excluded nor confirmed. We therefore carried out a new study with the aim of determining whether rotation of the infants' head to right or left sides affects the ventilation distribution in the two clinically relevant postures-supine and prone. We also studied an equally large group of mechanically ventilated infants using the same protocol to establish whether there are differences between the ventilation distributions in these two different types of ventilation.
Methods
Patients
Ten unsedated, nonintubated spontaneously breathing infants and ten mechanically ventilated infants were studied in the NICU. The study was approved by the University ethics committee, and informed written consent was obtained from the parents. The measurements were conducted according to the Declaration of Helsinki.
Basic characteristics of the infants are presented in Table 1. All infants were free of respiratory disease and required intensive care and mechanical ventilation for other diseases. In the spontaneously breathing group, the most frequent reason for admission to the NICU was suspected intrauterine infection (see Electronic Supplementary Material, ESM, S.T1). The most frequent diagnosis in the second group was congenital hernia (see ESM, S.T2). Four of the spontaneously breathing infants and six of the ventilated ones were prematurely born. Five infants from the former group and three from the latter were delivered by cesarean section.
Electrical impedance tomography
EIT was used to determine the distribution of lung ventilation. The EIT technique has frequently been described (e.g., [18, 19]). Briefly, the measuring principle of EIT is based on rotating injection of very small electrical currents and measurement of potential differences through a set of electrodes attached on the chest circumference. Each cycle of current injections and voltage measurements produces one scan of the instantaneous distribution of electrical impedance in the chest. Relative values showing the changes in local impedance with respect to a reference value (the average local impedance calculated over several consecutive breaths) are shown.
In our study EIT measurements were performed with the 16-electrode Göttingen GoeMF II system (Viasys Healthcare, Höchberg, Germany) [20, 21]. Electrical currents of 5 mArms and 50 kHz were used. EIT data were repeatedly acquired at 60-s intervals. The scan rate was 13 scans/s with a scan resolution of 32 × 32 pixels.
Protocol
The spontaneously breathing infants were examined approx. 30 min postprandially on their last day in the NICU before their discharge from hospital. The ventilated infants were studied immediately after their transfer from the operating room to the NICU. They were intubated via the nasotracheal route and ventilated in the pressure-controlled continuous positive pressure ventilation mode (Babylog 8000, Drägerwerk, Lübeck, Germany).
Sixteen ECG electrodes (Blue Sensor BR-50-K, Ambu, Friedberg, Germany) were placed on the chest circumference. (In the mechanically ventilated infants the electrodes were attached in the operating room to minimize the handling time in the NICU.) The electrodes were connected to the EIT device. The infants were randomly assigned to a supine/prone or prone/supine examination sequence combined with different head positions. The following combinations were studied: supine with head in the midline position (SM), supine with head turned to the right (SR), supine with head turned to the left (SL), prone with head turned to the right (PR), and prone with head turned to the left (PL).
The examination lasted approx. 40 min in the spontaneously breathing group and 20 min in the artificially ventilated one. The spontaneously breathing infants were unsedated; therefore occasional stretching or crawling movements occurred during the measurements. For this reason a higher number of EIT measurements was performed in this group resulting in a longer total examination time. (The measurements were repeated between three and five times in the spontaneously breathing and two or three times in the mechanically ventilated infants.) During the measurements no care procedures were allowed, and no adjustments of the ventilator settings were made.
Off-line data analysis
In each infant and body/head position studied six short EIT data sequences comprising four to six consecutive breaths were selected from the 60-s EIT recordings. The following selection criteria were used during tidal breathing: (a) regular breathing rate, (b) stable tidal and end-expiratory lung volume, and (c) no body, head, or arm movement. During mechanical ventilation no special selection criteria had to be used because the ventilatory pattern was stable and the infants did not move. The data were low-pass filtered with a cutoff frequency of 2 Hz.
The short data sequences were analyzed as follows: first, the end-inspiratory maximum and the end-expiratory minimum values of relative impedance change were identified and the average differences between these values calculated in all image pixels (Fig. 1, right). These ventilation related impedance changes were depicted in the corresponding pixels in different gray tones depending on their magnitude (i.e., the largest values were shown in white and the smallest in black). The light areas in such functional scans show the ventilated lung regions (Fig. 1, left). The next data evaluation step summed the pixel values of ventilation related impedance changes in the right and left lung regions proportional to regional tidal volume. The regions were defined using a procedure described elsewhere [22]. The sum of ventilation related impedance changes in the right lung region divided by the sum of these values in both lung regions gave the fractional ventilation of the right lung in the chest cross-section studied. In each body/head position all six short sequences of EIT data selected were analyzed in the described manner and average values determined.
Functional EIT scan of regional lung ventilation (left) generated from the EIT data obtained during six consecutive breaths in a mechanically ventilated infant (patient 4). The ventilator settings were: tidal volume 13 ml, respiratory rate 25 breaths/min, positive end-expiratory pressure 3 mbar, peak inspiratory pressure 24 mbar, inspiration/expiration time 1/3, fraction of O2 in inspired gas 0.3. The orientation of the ventilation scan is the following: anterior is at the top and right side of the chest is on the left side of the image. The tracing of relative impedance change (right) shows a selected 15-s data segment in one of a total of 912 image pixels (cross exact location of the pixel). Gray, white arrows End-inspiratory maximum and end-expiratory minimum values needed for the determination of the ventilation related tidal change in local electrical impedance. The larger the local air volume change the larger is the local ventilation related impedance change and the lighter appears the corresponding area in the functional EIT ventilation scan
Results in the text and figures are presented as means ± SD of ten infants. The data from the spontaneously breathing and mechanically ventilated groups were compared using the paired Wilcoxon rank sum test. One-way analysis of variance and Student's paried t test were used for comparisons within each group. Two-tailed p values less than 0.05 were considered statistically significant.
Results
The quantitative analysis was performed on data sequences originating from several consecutive breaths. The number of breaths analyzed was comparable between the groups (Table 2). In the scans the right lung region was always larger than the left one. The region area was unaffected by the body/head position except for the right lung region which was larger in the SL, PR, and PL positions than in the SC during spontaneous breathing (Table 2). The spontaneously breathing infants had a higher respiratory rate than the ventilated ones (Table 2). No significant differences between the respiratory rates in the five body/head positions were observed. The mechanically ventilated infants were ventilated with the following settings: tidal volume 29 ± 13 ml, positive end-expiratory pressure 3.2 ± 1.2 mbar, peak inspiratory pressure 21.7 ± 2.6 mbar, inspiration/expiration time 1/3.2 ± 0.7 s, fraction of O2 in inspired gas 0.28 ± 0.04. There were no significant differences in the heart rates within or between the two groups (Table 2).
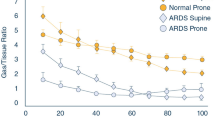
The sums of ventilation related impedance change in the right and left lung regions in spontaneously breathing and mechanically ventilated infants are given in Fig. 2. The tidal volumes in the right lung region (Fig. 2a) were significantly higher during mechanical than during spontaneous tidal ventilation. They were unaffected by body or head position. In prone infants the tidal volumes in the right lung region were significantly higher than in the left one. The tidal volumes in the left lung region (Fig. 2b) were also higher during mechanical than during spontaneous ventilation. However, in contrast with the right lung, their magnitude was influenced by the body and head position. During spontaneous breathing, this effect was more pronounced than during mechanical ventilation. Three combinations of body/head positions (SL, PR, PL) reduced the ventilation related changes in lung volume in the left lung region during spontaneous breathing when compared with the SM position. During artificial ventilation only the PL position exhibited this effect. These changes in regional tidal volumes had an impact on the right-to-left distribution of air between the two lung regions (Fig. 3) leading to an increase in fractional ventilation of the right lung in the SL, PR and PL positions during tidal breathing and in the PL position during mechanical ventilation. In both types of ventilation studied the largest effect was observed in the PL position.
Sum of ventilation related impedance change in the right (a) and left lung region (b) in mechanically ventilated and spontaneously breathing infants studied in different postures and head positions (means ± SD). SM supine position with the head in the neutral midline position, SR supine position with the head turned to the right side, SL supine position with the head turned to the left side, PR prone position with the head turned to the right side, PL prone position with the head turned to the left side, Z electrical impedance. *p < 0.05, **p < 0.01, ***p < 0.001 above means between mechanically ventilated and spontaneously breathing infants; *p < 0.05, **p < 0.01, ***p < 0.001 upper, lower parts (b) within the mechanically ventilated and spontaneously breathing groups; § p < 0.05, §§ p < 0.01 higher values in the right than in the left lung region
Discussion
Our study demonstrates significant effects of head/body position on the distribution of inspired air between the right and left lung regions during spontaneous tidal breathing. The higher fractional ventilation of the right lung in the chest cross-section in the prone posture was also found in our previous study [15]. The current examinations confirmed that the reduction in left lung tidal volumes occurred when the infants' heads were turned both to the right and left sides whereby the leftward rotation had a significantly higher effect. The rotation of the head to the left side reduced the tidal volumes in the left lung region and increased the fractional ventilation of the right lung also in the supine posture, although to a lesser degree. We did not expect the head position to have an influence on the right-to-left ventilation distribution during controlled mechanical ventilation. However, the effect of the leftward head rotation was observed in the prone posture even during this type of ventilation. All positions other than PL had no effect during artificial ventilation.
To our knowledge, such findings related to the distribution of regional ventilation in the lungs of neonates free of respiratory disease have not been reported before. Because of the methodological limitations addressed above, until recently almost no ethically justifiable methods existed that could have been used in this population in studies focusing on regional lung function. Thus the introduction of EIT opens up new possibilities in visualizing and quantifying regional lung ventilation in infants. Nevertheless, the present study does not allow the identification of the causative factors of this new phenomenon. We speculate that the leftward rotation of the head leads to some modification in the tissue and organ locations within the mediastinum with possible reduction in the gas flow into the left main and/or principal bronchi. The fact that rotation of the head to the left side affected the ventilation distribution even during mechanical ventilation seems to be supportive of such a mechanical, tractional effect. Nonetheless it is difficult to totally exclude some artifactual changes in the EIT images when organs move within the thorax.
The larger angle of divergence of the left than the right main stem bronchus from the trachea [23] may influence regional ventilation distribution. A postmortem study performed on intubated newborn infants revealed that the positioning of infants' heads to the right facilitated catheterization of the left main bronchus. In the straight head position and during leftward head rotation the catheterization of the right main stem bronchus dominated [23]. These primarily anatomical results cannot be directly compared with our dynamic functional data. Nevertheless, they provide a hint that the head position has an effect on the anatomical situation near the trachea bifurcation.
In spontaneously breathing infants the prone posture may have had an additional effect on regional tidal volumes in the caudal regions of the left lung caused by the changed diaphragmatic movement. The human newborn diaphragm is less effective in terms of its ability to compress gastric content and expand lower thorax because of its flatter configuration and narrower zone of apposition [24]. The prone body position would therefore be expected to affect the regional excursions of the diaphragm mainly near the stomach. This may explain why the ventilation redistribution was more pronounced in the spontaneously than in the mechanically ventilated neonates.
Because of the measuring principle of EIT, which is based on using small alternating currents, the EIT scans represent a slice of the chest, not a single transverse plane. (Unlike ionizing radiation, which passes straight through the body, the passage of electrical current is not confined to a two-dimensional plane.) Therefore impedance changes occurring out of the plane also contribute to the resulting EIT scan, although to a lesser degree than those taking place directly within the plane. This effect of the third dimension on the EIT scans has previously been studied [25]. Therefore the results of our study mainly reflect regional inequalities in ventilation distribution in the caudal lung regions in a chest slice lying below the electrodes and not in the apical zones which also may have been affected by the head/body position changes.
The EIT signal reflects all changes in electrical impedance occurring in the chest. Therefore not only the large impedance changes associated with lung ventilation but also the much smaller impedance changes associated with lung perfusion were detected. Several off-line data evaluation steps ensured that the results reflected only ventilation and not cardiac or perfusion related changes: (a) The EIT data were low-pass filtered; thus impedance changes synchronous with heart rate were excluded from analysis. (b) The analysis was performed only within the lung regions (not within the cardiac and mediastinum regions). (c) The data were analyzed in terms of end-inspiratory to end-expiratory impedance differences representative of tidal gas volume changes.
The effects of head position on lung ventilation have hardly been studied in infants. Postural effects have been followed more frequently, however, with partly conflicting findings. In the prone position no effect of postural change on the respiratory rate was found [26], there was reduced thoracoabdominal incoordination [26], fewer apneas, and less periodic breathing [27]. Increased airway resistance as well as lower peak flow rates and lung volumes were also found in the prone posture [28]. In the latter study the prone infants were only studied with their heads turned to the left (i.e., in the position which mainly affected regional ventilation distribution in our study) and compared with the supine posture with straight head position. Thus the study design did not allow the changes in lung mechanics to be attributed solely to the change in posture because the head position also may have had an effect. Rehan et al. [29] described significant differences between the diaphragm resting length and shortening at the level of the zone of apposition between the supine and prone postures. Unfortunately, the measurements were only performed on the right hemithorax. Thus they cannot provide information on any differences in the diaphragmatic excursions between the right and left sides of the body which might have helped to elucidate the mechanisms leading to the regionally dissimilar ventilation found in various body/head positions in our study.
Baird et al. [30] indirectly confirm the validity of our findings. They used plain transthoracic electrical impedance measurement to determine the breath amplitudes of the impedance signal in the supine and prone postures. This technique, nowadays routinely used for the respiratory rate monitoring in a clinical setting, utilizes the same basic measuring principle as EIT without providing any spatial information. Significantly lower breath amplitudes of transthoracic electrical impedance were found in the prone than in the supine posture. Our results also revealed this reduced magnitude of the ventilation related impedance change between inspiration and expiration in the prone posture and found that these changes occurred mainly in the left lung.
Our study identified new physiological phenomena in regional lung ventilation in spontaneously breathing and mechanically ventilated infants with no pulmonary disease as a result of head and body position changes. The scientific discussion on the favorable or unfavorable body positions in small infants is still going on. Because of the association between the prone sleeping position and sudden infant death syndrome (e.g., [17, 31, 32]) with no clearly identified causative mechanism [33] this issue is still topical. Our study provides new input into this discussion by addressing not only the effects of the body but also of the head position.
References
Schibler A, Hall GL, Businger F, Reinmann B, Wildhaber JH, Cernelc M, Frey U (2002) Measurement of lung volume and ventilation distribution with an ultrasonic flow meter in healthy infants. Eur Respir J 20:912–918
Aurora P, Gustafsson P, Bush A, Lindblad A, Oliver C, Wallis CE, Stocks J (2004) Multiple breath inert gas washout as a measure of ventilation distribution in children with cystic fibrosis. Thorax 59:1068–1073
Pillow JJ, Frerichs I, Stocks J (2006) Lung function tests in neonates and infants with chronic lung disease: global and regional ventilation inhomogeneity. Pediatr Pulmonol 41:105–121
Frerichs I, Braun B, Dudykevych T, Hahn G, Genée D, Hellige G (2004) Distribution of ventilation in young and elderly adults determined by electrical impedance tomography. Respir Physiol Neurobiol 143:63–75
Riedel T, Richards T, Schibler A (2005) The value of electrical impedance tomography in assessing the effect of body position and positive airway pressures on regional lung ventilation in spontaneously breathing subjects. Intensive Care Med 31:1522–1528
Smallwood RH, Hampshire AR, Brown BH, Primhak RA, Marven S, Nopp P (1999) A comparison of neonatal and adult lung impedances derived from EIT images. Physiol Meas 20:401–413
van Genderingen HR, Vugt AJ, Jansen JRC (2003) Estimation of regional lung volume changes by electrical impedance tomography during a pressure-volume maneuver. Intensive Care Med 29:233–240
Frerichs I, Hinz J, Herrmann P, Weisser G, Hahn G, Dudykevych T, Quintel M, Hellige G (2002) Detection of local lung air content by electrical impedance tomography compared with electron beam CT. J Appl Physiol 93:660–666
Hinz J, Neumann P, Dudykevych T, Andersson LG, Wrigge H, Burchardi H, Hedenstierna G (2003) Regional ventilation by electrical impedance tomography: a comparison with ventilation scintigraphy in pigs. Chest 124:314–322
Kunst PW, Vonk Noordegraaf A, Hoekstra OS, Postmus PE, de Vries PM (1998) Ventilation and perfusion imaging by electrical impedance tomography: a comparison with radionuclide scanning. Physiol Meas 19:481–490
Victorino JA, Borges JB, Okamoto VN, Matos GFJ, Tucci MR, Caramez MPR, Tanaka H, Sipmann FS, Santos DCB, Barbas CSV, Carvalho CRR, Amato MBP (2004) Imbalances in regional lung ventilation. A validation study on electrical impedance tomography. Am J Respir Crit Care Med 169:791–800
Caples M, Hubmayr RD (2003) Respiratory monitoring tools in the intensive care unit. Curr Opin Crit Care 9:230–235
Frerichs I, Schiffmann H, Hahn G, Hellige G (2001) Non-invasive radiation-free monitoring of regional lung ventilation in critically ill infants. Intensive Care Med 27:1385–1394
Wolf GK, Arnold JA (2005) Noninvasive assessment of lung volume: respiratory inductance plethysmography and electrical impedance tomography. Crit Care Med 33:S163–S169
Frerichs I, Schiffmann H, Ohler R, Dudykevych T, Hahn G, Hinz J, Hellige G (2003) Distribution of lung ventilation in spontaneously breathing neonates lying in different body positions. Intensive Care Med 29:787–794
Carlo WA, Beoglos A, Siner BS, Martin RJ (1989) Neck and body position effects on pulmonary mechanics in infants. Pediatrics 84:670–674
Paluszynska DA, Harris KA, Thach BT (2004) Influence of sleep position experience on ability of prone-sleeping infants to escape from asphyxiating microenvironments by changing head position. Pediatrics 114:1634–1639
Brown BH (2003) Electrical impedance tomography (EIT): a review. J Med Eng Technol 27:97–108
Frerichs I (2000) Electrical impedance tomography (EIT) in applications related to lung and ventilation: a review of experimental and clinical activities. Physiol Meas 21:R1–R21
Hahn G, Thiel F, Dudykevych T, Frerichs I, Gersing E, Schröder T, Hartung C, Hellige G (2001) Quantitative evaluation of the performance of different electrical tomography devices. Biomed Tech (Berl) 46:91–95
Hahn G, Dudykevych T, Frerichs I, Thiel F, Hellige G (2002) A high performance electrical impedance tomography (EIT) system for clinical evaluation studies and space application. In: Hutten H, Krösl P (eds) Proceedings of the 2nd European Medical & Biological Engineering Conference. Verlag der TU Graz, Graz, pp 110–111
Kühnel G, Hahn G, Frerichs I, Schröder T, Hellige G (1997) New methods for improving the image quality of functional electrical impedance tomography. Biomed Tech (Berl) 42 [Suppl]:470–471
Fewell J, Arrington R, Seibert J (1979) The effect of head position and angle of tracheal bifurcation on bronchus catheterization in the intubated neonate. Pediatrics 64:318–320
Woodrum D (1992) Respiratory muscles. In: Polin RA, Fox WW (eds) Fetal and neonatal physiology. Saunders, Philadelphia, pp 829–841
Rabbani KS, Kabir AM (1991) Studies on the effect of the third dimension on a two-dimensional electrical impedance tomography system. Physiol Meas 12:393–402
Adams JA, Zabaleta IA, Sackner MA (1994) Comparison of supine and prone non-invasive measurements of breathing patterns in fullterm newborns. Pediatr Pulmonol 18:8–12
Heimler R, Langlois J, Hodel DJ, Nelin LD, Sasidharan P (1992) Effect of positioning on the breathing pattern of preterm infants. Arch Dis Child 67:312–314
Shen XM, Zhoa W, Huang DS, Lin FG, Wu SM (1996) Effect of positioning on pulmonary function of newborns: comparison of supine and prone position. Pediatr Pulmonol 21:167–170
Rehan VK, Nakashima JM, Gutman A, Rubin LP, McCool FD (2000) Effects of the supine and prone position on diaphragm thickness in healthy term infants. Arch Dis Child 83:234–238
Baird TM, Neuman MR (1991) Effect of infant position on breath amplitude measured by transthoracic impedance and strain gauges. Pediatr Pulmonol 10:52–56
Alexander RT, Radisch D (2005) Sudden infant death syndrome risk factors with regards to sleep position, sleep surface, and co-sleeping. J Forensic Sci 50:147–151
Wells D, Gillies D, Fitzgerald D (2005) Positioning for acute respiratory distress in hospitalised infants and children. Cochrane Database Syst Rev 2:CD003645
Malloy MH (2004) SIDS-a syndrome in search of a cause. N Engl J Med 2:957–959
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is discussed in the editorial available at: http://dx.doi.org/10.1007/s00134-006-0253-z
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Heinrich, S., Schiffmann, H., Frerichs, A. et al. Body and head position effects on regional lung ventilation in infants: an electrical impedance tomography study. Intensive Care Med 32, 1392–1398 (2006). https://doi.org/10.1007/s00134-006-0252-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0252-0