Abstract
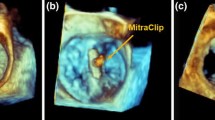
Mastering the technical skills required to perform pediatric cardiac valve surgery is challenging in part due to limited opportunity for practice. Transformation of 3D echocardiographic (echo) images of congenitally abnormal heart valves to realistic physical models could allow patient-specific simulation of surgical valve repair. We compared materials, processes, and costs for 3D printing and molding of patient-specific models for visualization and surgical simulation of congenitally abnormal heart valves. Pediatric atrioventricular valves (mitral, tricuspid, and common atrioventricular valve) were modeled from transthoracic 3D echo images using semi-automated methods implemented as custom modules in 3D Slicer. Valve models were then both 3D printed in soft materials and molded in silicone using 3D printed “negative” molds. Using pre-defined assessment criteria, valve models were evaluated by congenital cardiac surgeons to determine suitability for simulation. Surgeon assessment indicated that the molded valves had superior material properties for the purposes of simulation compared to directly printed valves (p < 0.01). Patient-specific, 3D echo-derived molded valves are a step toward realistic simulation of complex valve repairs but require more time and labor to create than directly printed models. Patient-specific simulation of valve repair in children using such models may be useful for surgical training and simulation of complex congenital cases.








Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- 2D:
-
Two-dimensional
- 3DE:
-
Three-dimensional echocardiogram
- Echo:
-
Echocardiogram
- DICOM:
-
Digital imaging in medicine
- CAVC:
-
Complete atrioventricular canal
- HLHS:
-
Hypoplastic left heart syndrome
References
Carpentier A, Chauvaud S, Mace L, Relland J, Mihaileanu S, Marino JP, Abry B, Guibourt P (1988) A new reconstructive operation for Ebstein’s anomaly of the tricuspid valve. J Thorac Cardiovasc Surg 96(1):92–101
Chauvaud S, Perier P, Touati G, Relland J, Kara SM, Benomar M, Carpentier A (1986) Long-term results of valve repair in children with acquired mitral valve incompetence. Circulation 74(3 Pt 2):I104–I109
Galloway AC, Colvin SB, Baumann FG, Esposito R, Vohra R, Harty S, Freeberg R, Kronzon I, Spencer FC (1988) Long-term results of mitral valve reconstruction with Carpentier techniques in 148 patients with mitral insufficiency. Circulation 78(3 Pt 2):I97–I105
Mahmood F, Matyal R (2015) A quantitative approach to the intraoperative echocardiographic assessment of the mitral valve for repair. Anesth Analg 121(1):34–58. https://doi.org/10.1213/ANE.0000000000000726
Poelaert JI, Bouchez S (2016) Perioperative echocardiographic assessment of mitral valve regurgitation: a comprehensive review. Eur J Cardiothorac Surg 50(5):801–812. https://doi.org/10.1093/ejcts/ezw196
Carpentier A, Branchini B, Cour JC, Asfaou E, Villani M, Deloche A, Relland J, D’Allaines C, Blondeau P, Piwnica A, Parenzan L, Brom G (1976) Congenital malformations of the mitral valve in children: pathology and surgical treatment. J Thorac Cardiovasc Surg 72(6):854–866
Baird CW, Myers PO, Marx G, Del Nido PJ (2012) Mitral valve operations at a high-volume pediatric heart center: Evolving techniques and improved survival with mitral valve repair versus replacement. Ann Pediatr Cardiol 5(1):13–20. https://doi.org/10.4103/0974-2069.93704
Rogers-Vizena CR, Sporn SF, Daniels KM, Padwa BL, Weinstock P (2016) Cost-benefit analysis of three-dimensional craniofacial models for midfacial distraction: a pilot study. Cleft Palate Craniofac J. https://doi.org/10.1597/15-281
Weinstock P, Prabhu SP, Flynn K, Orbach DB, Smith E (2015) Optimizing cerebrovascular surgical and endovascular procedures in children via personalized 3D printing. J Neurosurg Pediatr. https://doi.org/10.3171/2015.3.PEDS14677
Helder MR, Rowse PG, Ruparel RK, Li Z, Farley DR, Joyce LD, Stulak JM (2016) Basic cardiac surgery skills on sale for $22.50: an aortic anastomosis simulation curriculum. Ann Thorac Surg 101(1):316–322. https://doi.org/10.1016/j.athoracsur.2015.08.005 (discussion 322)
Joyce DL, Dhillon TS, Caffarelli AD, Joyce DD, Tsirigotis DN, Burdon TA, Fann JI (2011) Simulation and skills training in mitral valve surgery. J Thorac Cardiovasc Surg 141(1):107–112. https://doi.org/10.1016/j.jtcvs.2010.08.059
Yoo SJ, Spray T, Austin EH 3rd, Yun TJ, van Arsdell GS (2017) Hands-on surgical training of congenital heart surgery using 3-dimensional print models. J Thorac Cardiovasc Surg 153(6):1530–1540. https://doi.org/10.1016/j.jtcvs.2016.12.054
Mahmood F, Owais K, Taylor C, Montealegre-Gallegos M, Manning W, Matyal R, Khabbaz KR (2014) Three-dimensional printing of mitral valve using echocardiographic data. JACC Cardiovasc Imaging 8(2):227–229. https://doi.org/10.1016/j.jcmg.2014.06.020
Muraru D, Veronesi F, Maddalozzo A, Dequal D, Frajhof L, Rabischoffsky A, Iliceto S, Badano LP (2016) 3D printing of normal and pathologic tricuspid valves from transthoracic 3D echocardiography data sets. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jew215
Witschey WR, Pouch AM, McGarvey JR, Ikeuchi K, Contijoch F, Levack MM, Yushkevick PA, Sehgal CM, Jackson BM, Gorman RC, Gorman JH 3rd (2014) Three-dimensional ultrasound-derived physical mitral valve modeling. Ann Thorac Surg 98 (2):691–694. https://doi.org/10.1016/j.athoracsur.2014.04.094
Olivieri LJ, Krieger A, Loke YH, Nath DS, Kim PC, Sable CA (2015) Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Soc Echocardiogr 28(4):392–397. https://doi.org/10.1016/j.echo.2014.12.016
Vukicevic M, Puperi DS, Jane Grande-Allen K, Little SH (2017) 3D printed modeling of the mitral valve for catheter-based structural interventions. Ann Biomed Eng 45(2):508–519. https://doi.org/10.1007/s10439-016-1676-5
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin JC, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, Buatti J, Aylward S, Miller JV, Pieper S, Kikinis R (2012) 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging 30(9):1323–1341. https://doi.org/10.1016/j.mri.2012.05.001
Knight DS, Grasso AE, Quail MA, Muthurangu V, Taylor AM, Toumpanakis C, Caplin ME, Coghlan JG, Davar J (2015) Accuracy and reproducibility of right ventricular quantification in patients with pressure and volume overload using single-beat three-dimensional echocardiography. J Am Soc Echocardiogr 28(3):363–374. https://doi.org/10.1016/j.echo.2014.10.012
Watanabe K, Hashimoto I, Ibuki K, Okabe M, Kaneda H, Ichida F (2015) Evaluation of right ventricular function using single-beat three-dimensional echocardiography in neonate. Pediatr Cardiol 36(5):918–924. https://doi.org/10.1007/s00246-015-1095-7
Schattke S, Wagner M, Hattasch R, Schroeckh S, Durmus T, Schimke I, Sanad W, Spethmann S, Scharhag J, Huppertz A, Baumann G, Borges AC, Knebel F (2012) Single beat 3D echocardiography for the assessment of right ventricular dimension and function after endurance exercise: intraindividual comparison with magnetic resonance imaging. Cardiovasc Ultrasound 10:6. https://doi.org/10.1186/1476-7120-10-6
Jolley MA, Ghelani SJ, Adar A, Harrild DM (2017) Three-dimensional mitral valve morphology and age-related trends in children and young adults with structurally normal hearts using transthoracic echocardiography. J Am Soc Echocardiogr 30(6):561–571. https://doi.org/10.1016/j.echo.2017.01.018
Pouch AM, Aly AH, Lasso A, Nguyen AV, Scanlan AB, McGowan FX, Fichtinger G, Gorman RC, Gorman JH, Yushkevich PA, Jolley MA (2017) Image segmentation and modeling of the pediatric tricuspid valve in hypoplastic left heart syndrome. Lect Notes Comput Sc 10263:95–105. https://doi.org/10.1007/978-3-319-59448-4_10
Kutty S, Colen T, Thompson RB, Tham E, Li L, Vijarnsorn C, Polak A, Truong DT, Danford DA, Smallhorn JF, Khoo NS (2014) Tricuspid regurgitation in hypoplastic left heart syndrome: mechanistic insights from 3-dimensional echocardiography and relationship with outcomes. Circ Cardiovasc Imaging 7(5):765–772. https://doi.org/10.1161/CIRCIMAGING.113.001161
Pouch AM, Xu C, Yushkevich PA, Jassar AS, Vergnat M, Gorman JH 3rd, Gorman RC, Sehgal CM, Jackson BM (2012) Semi-automated mitral valve morphometry and computational stress analysis using 3D ultrasound. J Biomech 45 (5):903–907. https://doi.org/10.1016/j.jbiomech.2011.11.033
Pouch AM, Wang H, Takabe M, Jackson BM, Gorman JH 3rd, Gorman RC, Yushkevich PA, Sehgal CM (2014) Fully automatic segmentation of the mitral leaflets in 3D transesophageal echocardiographic images using multi-atlas joint label fusion and deformable medial modeling. Med Image Anal 18(1):118–129. https://doi.org/10.1016/j.media.2013.10.001
Yamauchi T, Taniguchi K, Kuki S, Masai T, Noro H, Nishino M, Fujita S (2004) Evaluation of the mitral valve leaflet morphology after mitral valve reconstruction with a concept “coaptation length index”. J Card Surg 19(6):535–538. https://doi.org/10.1111/j.0886-0440.2004.200329.x
Pouch AM, Aly A, Lasso A, Nguyen AV, Scanlan A, McGowan F, Fichtinger G, Gorman R, Gorman J, Yushkevich PA, Jolley M (2017) Image segmentation and modeling of the pediatric tricuspid valve in hypoplastic left heart syndrome. Lect Notes Comput Sci. https://doi.org/10.1007/978-3-319-59448-4_10
da Silva JP, Baumgratz JF, da Fonseca L, Franchi SM, Lopes LM, Tavares GM, Soares AM, Moreira LF, Barbero-Marcial M (2007) The cone reconstruction of the tricuspid valve in Ebstein’s anomaly. The operation: early and midterm results. J Thorac Cardiovasc Surg 133(1):215–223. https://doi.org/10.1016/j.jtcvs.2006.09.018
Acknowledgements
We would like to thank the 3D core sonographers group at The Children’s Hospital of Philadelphia (CHOP) for their outstanding images as well as the 3D printing facility at CHOP and the congenital cardiac surgical fellows who tested the valves.
Funding
This work was supported by the Department of Anesthesia and Critical Care at The Children’s Hospital of Philadelphia, the National Institute of Biomedical Imaging and Bioengineering (NIBIB) (P41 EB015902), Cancer Care Ontario with funds provided by the Ontario Ministry of Health and Long-Term Care and the Natural Sciences and Engineering Research Council of Canada.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical Approval
All procedures performed on humans were in accordance with the ethical standards of the Children’s Hospital of Philadelphia and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Scanlan, A.B., Nguyen, A.V., Ilina, A. et al. Comparison of 3D Echocardiogram-Derived 3D Printed Valve Models to Molded Models for Simulated Repair of Pediatric Atrioventricular Valves. Pediatr Cardiol 39, 538–547 (2018). https://doi.org/10.1007/s00246-017-1785-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1785-4