Abstract
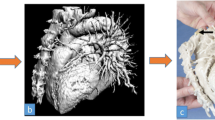
Improvements in technology and reduction in costs have led to widespread interest in three-dimensional (3D) printing. 3D-printed anatomical models contribute to personalized medicine, surgical planning, and education across medical specialties, and these models are rapidly changing the landscape of clinical practice. A physical object that can be held in one’s hands allows for significant advantages over standard two-dimensional (2D) or even 3D computer-based virtual models. Radiologists have the potential to play a significant role as consultants and educators across all specialties by providing 3D-printed models that enhance clinical care. This article reviews the basics of 3D printing, including how models are created from imaging data, clinical applications of 3D printing within the abdomen and pelvis, implications for education and training, limitations, and future directions.










Similar content being viewed by others
References
http://www.todaysmedicaldevelopments.com/article/3d-global-medical-market-2021-112916/. Cited 1 Jan 2017
Matsumoto JS, Morris JM, Foley TA, et al. (2015) Three-dimensional physical modeling : applications and experience at Mayo Clinic. Radiographics 35:1989–2006
Mitsouras D, Liacouras P, Imanzadeh A, et al. (2015) Medical 3D printing for the radiologist. Radiographics 35(7):1965–1988
Wake N, Rude T, Kang SK, et al. (2017) 3D printed renal cancer models derived from MRI data: application in pre-surgical planning. Abdom Radiol 42(5):1501–1509
Choy WJ, Mobbs RJ, Wilcox B, et al. (2017) Reconstruction of thoracic spine using a personalized 3D-printed vertebral body in adolescent with T9 primary bone tumor. World Neurosurg 105:1032.e13–1032.e17
Wong KC, Kumta SM, Geel NV, et al. (2015) One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg 20(1):14–23
Javan R, Herrin D, Tangestanipoor A (2016) Understanding spatially complex segmental and branch anatomy using 3D printing. Acad Radiol 23(9):1183–1189
Aranda JL, Jiménez MF, Rodríguez M, Varela G (2015) Tridimensional titanium-printed custom-made prosthesis for sternocostal reconstruction. Eur J Cardiothoracic Surg 48(4):e92–e94
Park E-K, Lim J-Y, Yun I-S, et al. (2016) Cranioplasty enhanced by three-dimensional printing. J Craniofac Surg 27(4):1
Bernhard J-C, Isotani S, Matsugasumi T, et al. (2016) Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World J Urol 34(3):337–345
Suzuki M, Ogawa Y, Kawano A, et al. (2004) Rapid prototyping of temporal bone for surgical training and medical education. Acta Otolaryngol 124(4):400–402
Adams F, Qiu T, Mark A, et al. (2017) Soft 3D-printed phantom of the human kidney with collecting system. Ann Biomed Eng 45(4):963–972
Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM (2014) Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. Anal Chem 86(7):3240–3253
Konno T, Mashiko T, Oguma H, et al. (2016) Rapid 3-dimensional models of cerebral aneurysm for emergency surgical clipping. No Shinkei Geka 44(8):651–660
Janusziewicz R, Tumbleston JR, Quintanilla AL, Mecham SJ, Desimone JM (2016) Layerless fabrication with continuous liquid interface production. Proc Natl Acad Sci USA 113(42):11703–11708
Ripley B, Levin D, Kelil T, et al. (2017) 3D printing from MRI Data: harnessing strengths and minimizing weaknesses. J Magn Reson Imaging 45(3):635–645
Hsu C, Ghaffari M, Alaraj A, et al. (2017) Gap-free segmentation of vascular networks with automatic image processing pipeline. Comput Biol Med 82(January):29–39
Schulz-Wendtland R, Harz M, Meier-Meitinger M, et al. (2017) Semi-automated delineation of breast cancer tumors and subsequent materialization using three-dimensional printing (rapid prototyping). J Surg Oncol 115(3):238–242
George E, Liacouras P, Rybicki FJ, Mitsouras D (2017) Measuring and establishing the accuracy and reproducibility of 3D printed medical models. Radiographics 5:160165
Leng S, McGee K, Morris J, et al. (2017) Anatomic modeling using 3D printing: quality assurance and optimization. 3D Print Med 3(1):6
Di Prima M, Coburn J, Hwang D, et al. (2015) Additively manufactured medical products—the FDA perspective. 3D Print Med 2(1):1
Zein NN, Hanouneh IA, Bishop PD, et al. (2013) Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transplant 19:1304–1310
Ikegami T, Maehara Y (2013) Transplantation: 3D printing of the liver in living donor liver transplantation. Nat Rev Gastroenterol Hepatol 10(12):697–698
Kong X, Nie L, Zhang H, et al. (2016) Do Three-dimensional visualization and three-dimensional printing improve hepatic segment anatomy teaching? A Randomized Controlled Study. J Surg Educ 73(2):264–269
Marro A, Bandukwala T, Mak W (2016) Three-dimensional printing and medical imaging: a review of the methods and applications. Curr Probl Diagn Radiol 45(1):2–9
Marconi S, Pugliese L, Del Chiaro M, et al. (2016) An innovative strategy for the identification and 3D reconstruction of pancreatic cancer from CT images. Updates Surg 68(3):273–278
Andolfi C, Plana A, Kania P, Banerjee PP, Small S (2017) Usefulness of three-dimensional modeling in surgical planning, resident training, and patient education. J Laparoendosc Adv Surg Tech 27(5):512–515
Sayed Aluwee SAZ, Bin Zhou X, Kato H, et al. (2017) Evaluation of pre-surgical models for uterine surgery by use of three-dimensional printing and mold casting. Radiol Phys Technol 10(3):279–285
Baek MH, Kim DY, Kim N, et al. (2016) Incorporating a 3-dimensional printer into the management of early-stage cervical cancer. J Surg Oncol 114(2):150–152
Werner H, Lopes J, Tonni G, Araujo Júnior E (2015) Physical model from 3D ultrasound and magnetic resonance imaging scan data reconstruction of lumbosacral myelomeningocele in a fetus with Chiari II malformation. Child’s Nerv Syst 31(4):511–513
Westerman ME, Matsumoto JM, Morris JM, Leibovich BC (2016) Three-dimensional printing for renal cancer and surgical planning. Eur Urol Focus 2(6):574–576
Silberstein JL, Maddox MM, Dorsey P, et al. (2014) Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: a pilot study. Urology 84(2):268–272
Zhang Y, Ge H, Li N, et al. (2016) Evaluation of three-dimensional printing for laparoscopic partial nephrectomy of renal tumors: a preliminary report. World J Urol 34(4):533–537
Wake N, Chandarana H, Huang WC, Taneja SS, Rosenkrantz AB (2016) Application of anatomically accurate, patient-specific 3D printed models from MRI data in urological oncology. Clin Radiol 71(6):610–614
Chen DYT, Uzzo RG (2009) Optimal management of localized renal cell carcinoma: surgery, ablation, or active surveillance. J Natl Compr Canc Netw 7(6):635–642; quiz 643
Sivarajan G, Huang WC (2012) Current practice patterns in the surgical management of renal cancer in the United States. Urol Clin N Am 39(2):149–160, v
Ellison JS, Montgomery JS, Hafez KS, et al. (2013) Association of RENAL nephrometry score with outcomes of minimally invasive partial nephrectomy. Int J Urol 20(6):564–570
Simhan J, Smaldone MC, Tsai KJ, et al. (2011) Objective measures of renal mass anatomic complexity predict rates of major complications following partial nephrectomy. Eur Urol 60(4):724–730
Zargar H, Allaf ME, Bhayani S, et al. (2015) Trifecta and optimal perioperative outcomes of robotic and laparoscopic partial nephrectomy in surgical treatment of small renal masses: a multi-institutional study. BJU Int 116(3):407–414
Atug F, Castle EP, Woods M, Davis R, Thomas R (2006) Robotics in urologic surgery: an evolving new technology. Int J Urol 13(7):857–863
Knoedler M, Feibus AH, Lange A, et al. (2015) Individualized physical 3-dimensional kidney tumor models constructed from 3-dimensional printers result in improved trainee anatomic understanding. Urology 85(6):1257–1261
Maddox MM, Feibus A, Liu J, et al. (2017) 3D-printed soft-tissue physical models of renal malignancies for individualized surgical simulation: a feasibility study. J Robot Surg 12(1):27–33
Tran-Gia J, Schlogl S, Lassmann M (2016) Design and fabrication of kidney phantoms for internal radiation dosimetry using 3D printing technology. J Nucl Med 57(12):1998–2005
Department of Health and Human Services: Center for Disease Control and Prevention and NCI (2014) U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999–2011 Incidence and Mortality Web-based Report
Siegel RL, Miller KD, Jemal A (2017) Cancer Statistics, 2017. CA Cancer J Clin 67(1):7–30
Shin T, Ukimura O, Gill IS (2016) Three-dimensional printed model of prostate anatomy and targeted biopsy-proven index tumor to facilitate nerve-sparing prostatectomy. Eur Urol 69(2):377–379
Reis SP, Majdalany BS, AbuRahma AF, et al. (2017) ACR appropriateness criteria® pulsatile abdominal mass suspected abdominal aortic aneurysm. J Am Coll Radiol 14(5):S258–S265
Powell JT, Sweeting MJ, Ulug P, et al. (2017) Meta-analysis of individual-patient data from EVAR-1, DREAM, OVER and ACE trials comparing outcomes of endovascular or open repair for abdominal aortic aneurysm over 5 years. Br J Surg 104(3):166–178
Reise JA, Sheldon H, Earnshaw J, et al. (2010) Patient preference for surgical method of abdominal aortic aneurysm repair: postal survey. Eur J Vasc Endovasc Surg 39(1):55–61
Neequaye SK, Aggarwal R, Van Herzeele I, Darzi A, Cheshire NJ (2007) Endovascular skills training and assessment. J Vasc Surg 46(5):1055–1064
Torres IO, De Luccia N (2016) A simulator for training in endovascular aneurysm repair: the use of three dimensional printers. Eur J Vasc Endovasc Surg 54(2):247–253
Tam MD, Latham TR, Lewis M, et al. (2016) A pilot study assessing the impact of 3-D printed models of aortic aneurysms on management decisions in EVAR planning. Vasc Endovasc Surg 50(1):4–9
Taylor SM, Mills JL, Fujitani RM (1994) The juxtarenal abdominal aortic aneurysm. A more common problem than previously realized? Arch Surg 129(7):734–737
Hu Z, Li Y, Peng R, et al. (2016) Experience with fenestrated endovascular repair of juxtarenal abdominal aortic aneurysms at a single center. Medicine (Baltimore) 95(10):e2683
Starnes BW, Tatum B (2012) Early report from an investigator-initiated investigational device exemption clinical trial on physician-modified endovascular grafts. J Vasc Surg 58(2):311–317
Taher F, Falkensammer J, McCarte J, et al. (2017) The influence of prototype testing in three-dimensional aortic models on fenestrated endograft design. J Vasc Surg 65(6):1591–1597
Leotta DF, Starnes BW (2015) Custom fenestration templates for endovascular repair of juxtarenal aortic aneurysms. J Vasc Surg 61(6):1637–1641
Meess KM, Izzo RL, Dryjski ML, Curl RE, et al. (2017) 3D printed abdominal aortic aneurysm phantom for image guided surgical planning with a patient specific fenestrated endovascular graft system. In: Cook TS, Zhang J (eds) Proceedings of SPIE—the International Society for Optical Engineering. SPIE, Bellingham, p 101380P
Koleilat I, Jaeggli M, Ewing JA, et al. (2016) Interobserver variability in physician-modified endograft planning by comparison with a three-dimensional printed aortic model. J Vasc Surg 64(6):1789–1796
Huang J, Li G, Wang W, Wu K, Le T (2016) 3D printing guiding stent graft fenestration: a novel technique for fenestration in endovascular aneurysm repair. Vascular 25(4):442–446
Itagaki MW (2015) Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol 21(4):338–341
Yuan D, Luo H, Yang H, et al. (2017) Precise treatment of aortic aneurysm by three-dimensional printing and simulation before endovascular intervention. Sci Rep. 7(1):795
Ruiz S, Galarreta D, Antón R, Cazón A, Finol EA (2017) A methodology for developing anisotropic AAA phantoms via additive manufacturing. J Biomech 57:161–166
Marconi S, Pugliese L, Botti M, et al. (2017) Value of 3D printing for the comprehension of surgical anatomy. Surg Endosc 31(10):4102–4110
Waran V, Devaraj P, Hari Chandran T, et al. (2012) Three-dimensional anatomical accuracy of cranial models created by rapid prototyping techniques validated using a neuronavigation station. J Clin Neurosci 19(4):574–577
Mafeld S, Nesbitt C, Mccaslin J, et al. (2017) Three-dimensional (3D) printed endovascular simulation models: a feasibility study. Ann Transl Med 5(3):1–8
Kolesky DB, Truby RL, Gladman AS, et al. (2014) 3D bioprinting of vascularized, heterogeneous cell-laden tissue constructs. Adv Mater 26(19):3124–3130
Kang K, Kim Y, Lee SB, et al. (2017) Three-dimensional bio-printing of hepatic structures with direct-converted hepatocyte-like cells. Tissue Eng Part A . https://doi.org/10.1089/ten.TEA.2017.0161
Laronda MM, Rutz AL, Xiao S, et al. (2017) A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat Commun 8:15261
Huotilainen E, Jaanimets R, Valášek J, et al. (2014) Inaccuracies in additive manufactured medical skull models caused by the DICOM to STL conversion process. J Craniomaxillofac Surg 42(5):259–265
Hoang D, Perrault D, Stevanovic M, Ghiassi A (2016) Surgical applications of three-dimensional printing: a review of the current literature and how to get started. Ann Transl Med 4(23):456
http://3dprint.com/13033/stratasys-3d-printers-surgery/. Cited 5 Apr 2017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Bastawrous, S., Wake, N., Levin, D. et al. Principles of three-dimensional printing and clinical applications within the abdomen and pelvis. Abdom Radiol 43, 2809–2822 (2018). https://doi.org/10.1007/s00261-018-1554-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1554-8