Abstract
Background
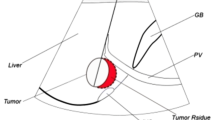
The dual-electrode bipolar-RFA (B-RFA) is increasingly used to ablate large liver tumours (3–7 cm). However, the challenging aspect of B-RFA is the placement of the two electrodes around the tumour. Realignment often requires the electrodes to be extracted and reinserted.
Aim
The aim of this study is to examine “Edgeboost”, a novel technique to increase the lateral ablation dimension without requiring any realignment of the electrodes.
Methods and Materials
An egg-white model and an ex vivo calf liver model were used compare the standard bipolar mode ablation to Edgeboost-1 (reaching full impedance in bipolar mode initially, then cycling in unipolar mode between left and right probes) and Edgeboost-2 (similar to Edgeboost-1 but not reaching full impedance initially in bipolar mode in order to minimize charring and, thus, to increase total ablation time).
Results
A significantly larger outer lateral ablation dimension to the probe was achieved with Edgeboost-1 compared to the standard method in the liver model (1.14 cm, SD: 0.16 vs. 0.44 cm, SD: 0.24, p = 0.04). Edgeboost-2 achieved the largest outer lateral ablation dimension of 1.75 cm (SD: 0.35). A similar association was seen in the egg model. Edgeboost-2 almost doubled the mass ablated with standard bipolar alone (mass ratio: 1:1.94 in egg white and 1:1.84 in liver).
Conclusion
This study demonstrates that the novel “Edgeboost” technique can increase the outer lateral ablation dimension without requiring the two inserted electrodes to be reinserted. This would be beneficial for interventionists who use the dual B-RFA.






Similar content being viewed by others
References
Lau WY, Lai EC. The current role of radiofrequency ablation in the management of hepatocellular carcinoma: a systematic review. Ann Surg. 2009;249:20–5.
Garrean S, Hering J, Saied A, Helton WS, Espat NJ. Radiofrequency ablation of primary and metastatic liver tumors: a critical review of the literature. Am J Surg. 2008;195:508–20.
Duffy JP, Hiatt JR, Busuttil RW. Surgical resection of hepatocellular carcinoma. Cancer J. 2008;14:100–10.
Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001;13:129.
Abitabile P, Hartl U, Lange J, Maurer CA. Radiofrequency ablation permits an effective treatment for colorectal liver metastasis. Eur J Surg Oncol. 2007;33(1):67–71.
Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–38.
Wong SL, Mangu Pamela B, Choti Michael A, et al. American Society of Clinical Oncology 2009 clinical evidence review on radiofrequency ablation of hepatic metastases from colorectal cancer. J Clin Oncol. 2010;28(3):493–508.
Evrard S, Becouarn Y, Fonck M, Brunet R, Mathoulin-Pelissier S, Picot. V. Surgical treatment of liver metastases by radiofrequency ablation, resection, or in combination. Eur J Surg Oncol. 2004;30(4):399–406.
Harrison LE, Koneru B, Baramipour P, et al. Locoregional recurrences are frequent after radiofrequency ablation for hepatocellular carcinoma. J Am Coll Surg. 2003;197:759–64.
Abdalla EK, Vauthey JN, Ellis LM, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004;239:818–25.
Yi B, Somasundar P, Espat NJ. Novel laparoscopic bipolar radiofrequency energy technology for expedited hepatic tumour ablation. HPB. 2009;11:135–9.
Flanders VL, Gervais DA. Ablation of liver metastases: current status. J Vasc Interv Radiol. 2010;21(Suppl):S214–22.
Ritz JP, Lehmann KS, Isbert C, et al. In vivo simulation of a novel bipolar radiofrquency device for interstitial thermotherapy of liver tumors during normal and interrupted hepatic perfusion. Surg Res. 2006;133:176–84.
Berjano FJ, Burdio F, Navarro AC, et al. Improved perfusion system for bipolar radiofrequency ablation of livers: preliminary findings from a computer modeling study. Physiol Meas. 2006;27:N55–66.
Burdio F, Navarro A, Sousa R, et al. Evolving technology in bipolar perfused radiofrequency ablation: assessment of efficacy, predictability, and safety in a pig liver model. Eur Radiol. 2006;16:1826–34.
Burdio F, Güemes A, Burdio JM, et al. Bipolar saline-enhanced electrode for radiofrequency ablation: results of experimental studies on in vivo porcine liver. Radiology. 2003;226:447–56.
Eisele RM, Neuhaus P, Schumacher G. Radiofrequency ablation of liver tumors using a novel bipolar device. J Laparoendosc Adv Surg Tech. 2008;18:857–63.
Pillai K, Akhter J, Chua TC, et al. Heat sink effect on tumor ablation characteristics as observed in monopolar radiofrequency, bipolar radiofrequency, and microwave, using ex vivo calf liver model. Medicine. 2015;94(9):1–10.
Haemmerich D, Staelin ST, Tungjitkusolmun S, Lee FTJ, Mahvi DM, Webster JG. Hepatic bipolar radio-frequency ablation between separated multiprong electrodes. Trans Biomed Eng. 2001;48:1145–52.
Jaskolka JD, Asch MR, Kachura JR, et al. Needle tract seeding after radiofrequency ablation of hepatic tumors. J Vasc Interv Radiol. 2005;16(4):485–91.
Nordlinger B, Benoist S. Treatment options for metastatic liver cancer. Surgical resection including perioperative chemotherapy (adjuvant and neoadjuvant). Eur J Cancer. 2003;1:181–8.
Jin GY, Park SH, Han YM, et al. Radio frequency ablation in the rabbit lung using wet electrodes: comparison of monopolar and dual bipolar electrode mode. Korean J Radiol. 2006;7:97–105.
Alemi F, Kwon E, Stewart L, Corvera CU. A comparison of monopolar to bipolar radiofrequency ablation of liver tumors. HPB. 2011;13:2–3.
McGahan JP, Brock JM, Tasluk H, et al. Hepatic ablation with use of radio-frequency electrocautery in the animal model. J Vasc Interv Radiol. 1992;3:291–6.
Organ LW. Electrophysiologic principles of radiofrequency lesion making. Appl Neurophysiol. 1976;39:69–76.
Chen MH, Yang W, Yan K, et al. Large liver tumors: protocol for radiofrequency ablation and its clinical application in 110 patients—mathematic model, overlapping mode, and electrode placement process. Radiology. 2004;232(1):260–71.
Collyer WC, Landman J, Olweny EO, et al. Comparison of renal ablation with cryotherapy, dry radiofrequency, and saline augmented radiofrequency in a porcine model. J Am Coll Surg. 2001;193:505.
Meijerink MR, Van Den Tol P, Van Tilborg AAJM, Van Waesberghe JHTM, Meijer S, Van Kuijk C. Radiofrequency ablation of large size liver tumours using novel plan-parallel expandable bipolar electrodes: initial clinical experience. Eur J Radiol. 2011;77(1):167–71.
Van Tilborg AA, Nielsen K, Scheffer HJ, et al. Bipolar radiofrequency ablation for symptomatic giant (>10 cm) hepatic cavernous haemangiomas: initial clinical experience. Clin Radiol. 2013;68(1):e9–14.
Haemmerich D, Wright AW, Mahvi DM, Lee FTJ, Webster JG. Hepatic bipolar radiofrequency ablation creates coagulation zones close to blood vessels: a finite element study. Med Biol Eng Comput. 2003;41:317.
Al-Alem I, Pillai K, Akhter J, Chua TC, Morris DL. Heat sink phenomenon of bipolar and monopolar radiofrequency ablation observed using polypropylene tubes for vessel simulation. Surg Innov. 2014;21(3):269–76.
Lee JM, Han JK, Kim SH, et al. Saline-enhanced hepatic radiofrequency ablation using a perfused-cooled electrode: comparison of dual probe bipolar mode with monopolar and single probe bipolar modes. Korean J Radiol. 2004;5(2):121–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Huo, Dr. Pillai, and Dr. Akhter have nothing to disclose. Dr. Morris reports other from RFA Medical, outside the submitted work; In addition, Dr. Morris has a patent Yes licenced to RFA Medical.
Research Involving Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Huo, Y.R., Pillai, K., Akhter, J. et al. “Edgeboost”: A Novel Technique to Extend the Ablation Zone Lateral to a Two-Probe Bipolar Radiofrequency Device. Cardiovasc Intervent Radiol 39, 97–105 (2016). https://doi.org/10.1007/s00270-015-1168-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1168-2