Abstract
Background
The potential of a tumour’s volumetric measures obtained from pretreatment MRI sequences of glioblastoma (GBM) patients as predictors of clinical outcome has been controversial. Mathematical models of GBM growth have suggested a relation between a tumour’s geometry and its aggressiveness.
Methods
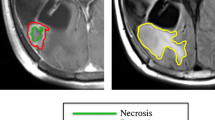
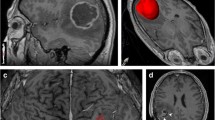
A multicenter retrospective clinical study was designed to study volumetric and geometrical measures on pretreatment postcontrast T1 MRIs of 117 GBM patients. Clinical variables were collected, tumours segmented, and measures computed including: contrast enhancing (CE), necrotic, and total volumes; maximal tumour diameter; equivalent spherical CE width and several geometric measures of the CE “rim”. The significance of the measures was studied using proportional hazards analysis and Kaplan-Meier curves.
Results
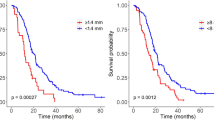
Kaplan-Meier and univariate Cox survival analysis showed that total volume [p = 0.034, Hazard ratio (HR) = 1.574], CE volume (p = 0.017, HR = 1.659), spherical rim width (p = 0.007, HR = 1.749), and geometric heterogeneity (p = 0.015, HR = 1.646) were significant parameters in terms of overall survival (OS). Multivariable Cox analysis for OS provided the later two parameters as age-adjusted predictors of OS (p = 0.043, HR = 1.536 and p = 0.032, HR = 1.570, respectively).
Conclusion
Patients with tumours having small geometric heterogeneity and/or spherical rim widths had significantly better prognosis. These novel imaging biomarkers have a strong individual and combined prognostic value for GBM patients.
Key Points
• Three-dimensional segmentation on magnetic resonance images allows the study of geometric measures.
• Patients with small width of contrast enhancing areas have better prognosis.
• The irregularity of contrast enhancing areas predicts survival in glioblastoma patients.




Similar content being viewed by others
Abbreviations
- GBM:
-
Glioblastoma
- PFS:
-
Progression-free Survival
- OS:
-
Overall survival
- KPS:
-
Karnofsky performance status
- VAK:
-
Volume-Age-KPS
- 3D:
-
Three-dimensional
- CE:
-
Contrast enhancing
- DICOM:
-
Digital imaging and communication in medicine
- VCE :
-
CE volume
- VI :
-
Inner volume
- V:
-
Total postcontrast T1 tumour volume
- dmax 3D:
-
Maximum tumour diameter in 3D
- δ s :
-
Average size of CE rim
- GH :
-
Measure of geometric heterogeneity of the CE rim width
- HR:
-
Hazard ratio
- 2D:
-
Bidimensional
- Gd:
-
Gadolinium
- p :
-
p-value
References
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Ellingson BM (2015) Radiogenomics and imaging phenotypes in glioblastoma: novel observations and correlation with molecular characteristics. Curr Neurol Neurosci Rep 15:506
Zinn PO, Mahmood Z, Elbanan MG, Colen RR (2015) Imaging Genomics in Gliomas. Cancer J 21:225–234
Wen PY, Macdonald DR, Reardon DA, Cloughesy TF, Sorensen AG, Galanis E et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972
Iliadis G, Selviaridis P, Kalogera-Fountzila A, Fragkoulidi A, Baltas D, Tselis N et al (2009) The importance of tumor volume in the prognosis of patients with glioblastoma: comparison of computerized volumetry and geometric models. Strahlenther Onkol 185:743–750
Mazurowski MA, Zhang J, Peters KB, Hobbs H (2014) Computer-extracted MR imaging features are associated with survival in glioblastoma patients. J Neurooncol 120:483–488
Zinn PO, Sathyan P, Mahajan B, Bruyere J, Hegi M, Majumder S et al (2012) A novel volume-age-KPS (VAK) glioblastoma classification identifies a prognostic cognate microRNA-gene signature. PLoS One 7:e41522
Mazurowski MA, Desjardins A, Malof JM (2013) Imaging descriptors improve the predictive power of survival models for glioblastoma patients. Neuro Oncol 15:1389–1394
Zacharaki EI, Morita N, Bhatt P, O'Rourke DM, Melhem ER, Davatzikos C (2012) Survival analysis of patients with high-grade gliomas based on data mining of imaging variables. AJNR Am J Neuroradiol 33:1065–1071
Pérez-García VM, Calvo GF, Belmonte-Beitia J, Diego D, Pérez-Romasanta LA (2011) Bright solitary waves in malignant gliomas. Phys Rev E 84:021921
Ellingson BM, Bendszus M, Boxerman J et al (2015) Consensus recommendations for a standardized Brain Tumor Imaging Protocol in clinical trials. Neuro Oncol 17:1188–1198
Goel MK, Khanna P, Kishore J (2010) Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res 1:274–278
Zhang Z, Jiang H, Chen X, Bai J, Cui Y, Ren X et al (2014) Identifying the survival subtypes of glioblastoma by quantitative volumetric analysis of MRI. J Neurooncol 119:207–214
Ramakrishna R, Barber J, Kennedy G, Rizvi Win RH, Ojemann GA, Berger MS et al (2010) Imaging features of invasion and preoperative and postoperative tumor burden in previously untreated glioblastomas: correlation with survival. Surg Neurol Int 1:40
Gutman DA, Cooper LA, Hwang SN et al (2013) MR imaging predictors of molecular profile and survival: multi-institutional study of the TCGA glioblastoma data set. Radiology 267:560–569
Wangaryattawanich P, Hatami R, Wang J et al (2015) Multicenter imaging outcomes study of The Cancer Genome Atlas glioblastoma patient cohort: imaging predictors of overall and progression-free survival. Neuro Oncol 17:1525–1537
Deisboeck DS, Guiot C, Delsanto PP, Pugno N (2006) Does cancer growth depend on surface extension? Med Hypotheses 67:1338–1341
Macyszyn L, Akbari H, Pisapia JM, Da X, Attiah M, Pigrish V, et al (2015) Imaging patterns predict patient survival and molecular subtype in glioblastoma via machine learning techniques. Neuro Oncol 18:417–425
Itakura H, Achrol AS, Mitchell LA, Loya JJ, Liu T, Westbroek EM et al (2015) Magnetic resonance image features identify glioblastoma phenotypic subtypes with distinct molecular pathway activities. Sci Transl Med 7:303ra138
Acknowledgments
We would like to acknowledge Juan Belmonte (Universidad de Castilla-La Mancha) for discussions. The scientific guarantor of this publication is Víctor M. Manuel Pérez-García (Victor.PerezGarcia@uclm.es), full professor and head of Department of Mathematics at Universidad de Castilla-La Mancha (Spain). The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This work has been supported by Ministerio de Economía y Competitividad/FEDER, Spain [grant numbers: MTM2012-31073 and MTM2015-71200-R], Consejería de Educación Cultura y Deporte from Junta de Comunidades de Castilla-La Mancha (Spain) [grant number PEII-2014-031-P] and James S. Mc. Donnell Foundation (USA) 21st Century Science Initiative in Mathematical and Complex Systems Approaches for Brain Cancer (Special Initiative Collaborative – Planning Grant 220020420 and Collaborative award 220020450). Complex statistical methods were necessary for this paper. Víctor M. Pérez-García, Alicia Martínez-González and David Molina (Matematicians) have significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: retrospective, observational, multicenter study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pérez-Beteta, J., Martínez-González, A., Molina, D. et al. Glioblastoma: does the pre-treatment geometry matter? A postcontrast T1 MRI-based study. Eur Radiol 27, 1096–1104 (2017). https://doi.org/10.1007/s00330-016-4453-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4453-9