Abstract
Background
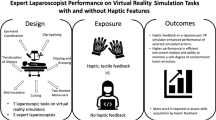
In the literature of skill acquisition and transfer of skills, it often is assumed that the rate of skill acquisition depends on what has been learned in a similar context (i.e., surgical simulators providing haptic feedback). This study aimed to analyze whether the addition of haptic feedback early in the training phase for image-guided surgical simulation improves performance.
Methods
A randomized crossover study design was used, in which 38 surgical residents were randomized to begin a 2-h simulator training session with either haptic or nonhaptic training followed by crossover after 1 h. The graphic context was a virtual upper abdomen. The residents performed two diathermy tasks. Two validated tests were used to control for differences in visual–spatial ability: the BasIQ general cognitive ability test and Mental Rotation Test A (MRT-A).
Results
After 2 h of training, the group that had started with haptic feedback performed the two diathermy tasks significantly better (p < 0.05, unpaired t-test). Only the group that had started with haptic training significantly improved during the last 1-h session (p < 0.01, paired t-test).
Conclusion
The findings indicate that haptic feedback could be important in the early training phase of skill acquisition in image-guided surgical simulator training.




Similar content being viewed by others

References
Ackerman PL (1992) Predicting individual differences in complex skill acquisition: dynamics of ability determinants. J Appl Psychol 77: 598–614
Basdogan C, De S, Kim J, Muniyandi M, Kim H, Srinivasan MA (2004) Haptics in minimally invasive surgical simulation and training. IEEE Computer Graphics Applications 24: 56–64
Berkley J, Turkiyyah G, Berg D, Ganter M, Weghorst S (2004) Real-time finite element modeling for surgery simulation: an application to virtual suturing. IEEE Transact Visualization Computer Graphics 10: 314–325
Bethea BT, Okamura AM, Kitagawa M, Fitton TP, Cattaneo SM, Gott VL, Baumgartner WA, Yuh DD (2004) Application of haptic feedback to robotic surgery. J Laparoendosc Adv Surg Tech A 14: 191–195
Bholat OS, Haluck RS, Kutz RH, Gorman PJ, Krummel TM (1999) Defining the role of haptic feedback in minimally invasive surgery. Stud Health Technol Inform 62: 62–66
Bholat OS, Haluck RS, Murray WB, Gorman PJ, Krummel TM (1999) Tactile feedback is present during minimally invasive surgery. J Am Coll Surg 189: 349–355
Biggs SJ, Srinivasan MA (2002) Haptic interfaces. In: Stanney KM (eds). Handbook of virtual environments: design, implementation, and applications. Lawrence Erlbaum Associates, Mahwah, NJ pp 93–115
Borg G (1998) Borg´s perceived exertion and pain scales. In: Cotton RT (ed) Human kinetics. Champaign, IL, pp 30–67
Burdea CG, Coiffet P (1994) Virtual reality technology. John Wiley & Sons, New York
Csikszentmihalyi M (1990) Flow: the psychology of optimal experience. Harper/Collins, New York pp 1–49
Darzi A (2000) Hand-assisted laparoscopic colorectal surgery. Surg Endosc 14: 999–1004
Darzi A, Mackay S (2001) Assessment of surgical competence. Qual Health Care 10(Suppl 2): ii64–ii9
Felländer-Tsai L, Kjellin A, Wredmark T, Ahlberg G, Anderberg B, Enochsson L, Hedman L, Johnson E, Mäkinen K, Ramel S, Ström P, Särnå L, Westman B (2004) Basic accreditation for invasive image-guided intervention: a shift of paradigm in high technology education, embedding performance criterion levels in advanced medical simulators in a modern educational curriculum. J Inform Technol Healthcare 3: 165–173
Gallagher AG, Richie K, McClure N, McGuigan J (2001) Objective psychomotor skills assessment of experienced, junior, and novice laparoscopists with virtual reality. World J Surg 25: 1478–1483
Ghani JA, Deshpande PD (1994) The characteristics and the experience of optimal flow in human-computer interaction. J Psychol 128: 381–391
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91: 146–150
Hoffman HG (1998) Physically touching virtual objects using tactile augmentation enhances the realism of virtual objects IEEE. Proceedings of the IEEE Virtual Reality Annual Symposium, Atlanta, GA
Jordan JA, Gallagher AG, McGuigan J, McClure N (2001) Virtual reality training leads to faster adaptation to the novel psychomotor restrictions encountered by laparoscopic surgeons. Surg Endosc 15: 1080–1084
Kitagawa M, Dokko D, Okamura AM, Yuh DD (2005) Effect of sensory substitution on suture-manipulation forces for robotic surgical systems. J Thorac Cardiovasc Surg 129: 151–158
Lathan CE, Tracey MR, Sebrechts MM, Clawson DM, Higgins GA (2002) Using virtual environments as training simulators: measuring transfer. In: Stanney KM (eds). Handbook of virtual environments: design, implementation, and applications. Lawrence Erlbaum Associates, Mahwah, NJ pp 414–434
Louis TA, Lavori PW, Bailar JC, Polansky M (1984) Crossover and self-controlled designs in clinical research. N Engl J Med 5: 24–31
Mårdberg B, Sjöberg A, Henrysson-Eidvall S (2000) BasIQ begåvningstest: manual. Psykologiförlaget AB, Stockholm, Sweden, pp 47–55
Moody L, Baber C, Arvanitis TN (2002) Objective surgical performance evaluation based on haptic feedback. Stud Health Technol Inform 85: 304–310
Moorthy K, Munz Y, Sarker SK, Darzi A (2003) Objective assessment of technical skills in surgery. BMJ 327: 1032–1037
Nakao M, Imanishi K, Kuroda T, Oyama H (2004) Practical haptic navigation with clickable 3D region input interface for supporting master-slave type robotic surgery. Stud Health Technol Inform 98: 265–271
Nelson TW, Bolia RS (2002) Technological considerations in the design of multisensory virtual environments: the virtual field of dreams will have to wait. In: Stanney KM (eds). Handbook of virtual environments: design, implementation, and applications. Lawrence Erlbaum Associates: Mahwah, NJ pp 301–311
Peters M, Laeng B, Latham K, Jackson M, Zaitouna R, Richardson C (2000) A redrawn Vanderberg and Kuse mental rotation test: different versions and factors that affect performance. Brain Cogn 28: 39–58
Popescu GV, Burdea CG, Treffitz H (2002) Multimodal interaction modelling. In: Stanney KM (eds). Handbook of virtual environments: design, implementation, and applications. Lawrence Erlbaum Associates: Mahwah, NJ pp 435–454
Prystowsky JB, Regehr G, Rogers DA, Loan JP, Hiemenz LL, Smith KM (1999) A virtual reality module for intravenous catheter placement. Am J Surg 177: 171–175
Salas E, Cannon-Bowers JA (2001) The science of training: a decade of progress. Annu Rev Psychol 52: 471–479
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236: 458–463, discussion 463–464
Stanney KM, Zyda M (2002) Environments in the 21st century: introductory chapter. In: Stanney KM (eds). Handbook of virtual environments: design, implementation, and applications. Lawrence Erlbaum Associates: Mahwah, NJ pp 1–14
Strom P, Kjellin A, Hedman L, Johnson E, Wredmark T, Fellander-Tsai L (2003) Validation and learning in the Procedicus KSA virtual reality surgical simulator. Surg Endosc 17: 227–231
Strom P, Kjellin A, Hedman L, Wredmark T, Fellander-Tsai L (2004) Training in tasks with different visual-spatial components does not improve virtual arthroscopy performance. Surg Endosc 18: 115–120
Wagner CR, Stylopoulos N, Howe RD (2002) The role of haptic feedback in surgery: analysis of blunt dissection. Proceedings of the 10th Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems (HAPTICS) 39: 68–74
Wanzel KR, Hamstra SJ, Anastakis DJ, Matsumoto ED, Cusimano MD (2002) Effect of visual–spatial ability on learning of spatially complex surgical skills. Lancet 359: 230–231
Wickens CD, Lee JD, Liu Y, Gordon Becker SE (2004) An introduction to human factors engineering. Pearson, Prentice Hall, NJ
Acknowledgments
This study was supported by research grants from Karolinska Institutet, Huddinge University Hospital AB, and the European Commission Goal 1: North of Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ström, P., Hedman, L., Särnå, L. et al. Early exposure to haptic feedback enhances performance in surgical simulator training: a prospective randomized crossover study in surgical residents. Surg Endosc 20, 1383–1388 (2006). https://doi.org/10.1007/s00464-005-0545-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0545-3