Abstract
Background
Laparoscopic surgery challenges both the surgical novice and experienced open surgeon with unique psychomotor adaptations. Surgical skills assessment has historically relied on subjective opinion and case experience. Objective performance metrics have stimulated much interest in surgical education over the last decade and proficiency-based simulation has been proposed as a paradigm shift in surgical skills training. New assessment tools must be subjected to scientific validation. This study examined the construct validity of a hybrid laparoscopic simulator with in-built motion tracking technology.
Methods
Volunteers were recruited from four experience groups (consultant surgeon, senior trainee, junior trainee, medical student). All subjects completed questionnaires and three tasks on the ProMIS laparoscopic simulator (laparoscope orientation, object positioning, sharp dissection). Motion analysis data was obtained via optical tracking of instrument movements. Objective metrics included time, path length (economy of movement), smoothness (controlled handling) and observer-recorded penalty scores.
Results
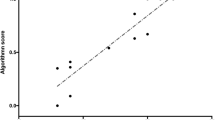
One hundred and sixty subjects completed at least one of the three tasks. Significant group differences were confirmed for number of years qualified, age and case experience. Significant differences were found between experts and novices in all three tasks. Sharp dissection was the strongest discriminator of four recognised laparoscopic skill groups: consultants outperformed students and juniors in all three performance metrics and objective penalty score (p < 0.05), and only accuracy of dissection did not distinguish them from senior trainees (p = 0.261). Seniors dissected faster, more efficiently and more accurately than juniors and students (p < 0.05).
Conclusions
ProMIS provides a construct valid laparoscopic simulator and is a feasible tool to assess skills in a cross-section of surgical experience groups. ProMIS has the potential to objectively measure pre-theatre dexterity practice until an agreed proficiency level of dexterity is achieved. Future work should now examine whether training to expert criterion levels on ProMIS correlates with actual operative performance.




Similar content being viewed by others
References
Carlin AM, Gasevic E, Shepard AD (2007) Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg 193:326–330
Chikwe J, de Souza A (2004) Pepper JR (2004) No time to train surgeons. BMJ 328:418–419
Heath RM, Gate T, Halloran C, Callaghan M, Paraoan M, Blair SD (2005) The European Working Time Directive ‘triple whammy’: hitting surgical trainees where it hurts. Br J Surg 92(Supp 1):113
Modernising Medical Careers: the response of the four UK Health Ministers to the consultation on Unfinished Business: Proposals for Reform of the Senior House Officer Grade. 26-2-0003
UK Health Departments. Modernising Medical Careers: the next steps. 15-4-2004. London, Department of Health
http://www.iscp.ac.uk. 2006
Paisley AM, Baldwin PJ, Patterson-Brown S (2001) Validity of surgical simulation for the assessment of operative skill. Br J Surg 88:1525–1532
Darzi A, Mackay S (2001) Assessment of surgical competence. Qual Health Care 10:ii64–ii69
Figert P, Park A, Witkze D, Schwartz R (2001) Transfer of training in acquiring laparoscopic skills. J Am Coll Surg 193:534–537
Satava RM (1993) Virtual reality surgical simulator: the first steps. Surg Endosc 7:203–205
Gallagher AG, Ritter EM, Champion HR, Higgins G, Fried GM, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
Gallagher AG, Ritter EM, Satava RM (2003) Fundamental principles of validation and reliability: rigorous science for the assessment of surgical education and training. Surg Endosc 17:1525–1529
Streiner D, Norman G (1989) Health measurement scales. New York, Oxford University Press
Derossis AM, Fried GM, Abrahamowicz MA, Sigman HH, Barkun JS, Meakins JL (1998) Development of a model for training and evaluation of laparoscopic skills. Am J Surg 175:482–487
Gallagher AG, Lederman AB, McGlade K, Satava RM, Smith CD (2004) Discriminitive validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST VR) using criteria levels based on expert performance. Surg Endosc 18:660–665
Schijven MP, Jakimowicz J (2003) Construct validity: experts and novices performing on the Xitact LS500 laparoscopy simulator. Surg Endosc 17:803–810
Royal College of Surgeons of England (2006) Inquiry into independent sector treatment centres. Ann R Coll Surg 88(Suppl):116–119
Cruelty to Animals Act. 39 and 40 Vict, 1–8. 1876. Ch77
Mahadevan V (2006) The Human Tissue Act 2004: implications for anatomical work at the college. Bulletin of the Royal College of Surgeons of England 88:264–265
Reznick R, MacRae H (2006) Teaching surgical skills—changes in the wind. N Engl J Med 355:2664–2669
Gaba D (2004) The future vision of simulation in healthcare. Qual Safety Healthcare 13:2–10
Kneebone R (2003) Simulation in surgical training: educational issues and practical implications. Med Educ 37:267–277
Scott D, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus D, Jeyarajah R, Thompson W (2000) Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience. J Am Coll Surg 191:272–283
Rosser JC, Rosser LE, Savalgi RS (1997) Skill acquisition and assessment for laparoscopic surgery. Arch Surg 132:200–204
Smith CD, Tung P (1998) Assessing laparoscopic manipulative skill: beyond the stopwatch. Surg Endosc 12:492
Schmidt R, Wrisberg C (2000) Motor Learning and Performance. Champaign, IL, Human Kinetics
Moynihan BGA (1920) Ritual of a surgical operation. Br J Surg 8:27–35
Adrales G, Donnelly M, Chu U, Witkze D, Hoskins J, Mastrangelo M Jr, Gandsas A, Park A (2004) Determinants of competency judgments by experienced laparoscopic surgeons. Surg Endosc 18:323–327
Martin J, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, Brown M (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84:273–278
Moorthy K, Munz Y, Dosis A, Bello F, Chang A, Darzi A (2004) Bimodal assessment of laparoscopic suturing skills: construct and concurrent validity. Surg Endosc 18:1608–1612
Broe D, Ridgway P, Johnson S, Tierney S, Conlon C (2006) Construct validation of a novel hybrid surgical simulator. Surg Endosc 20:900–904
Gallagher AG, Satava RM (2002) Virtual reality as a metric for the assessment of laparoscopic psychomotor skills. Surg Endosc 16:1746–1752
Gallagher AG, Smith CD, Bowers SP, Seymour NE, Pearson A, McNatt S, Hananel D, Satava RM (2003) Psychomotor skills assessment in practicing surgeons experienced in performing advanced laparoscopic procedures. J Am Coll Surg 197:479–488
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2003) Learning curves and impact of previous operative experience on performance on a virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185:146–149
Grantcharov TP, Rosenberg J, Pahle E, Funch-Jensen P (2001) Virtual reality computer simulation: an objective method for the evaluation of laparoscopic surgical skills. Surg Endosc 15:242–244
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Pearson A, Gallagher AG, Rosser JC, Satava RM (2002) Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc 16:130–137
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Anderson DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–464
Chaudhry A, Sutton C, Wood J, Stone R, McCloy R (1999) Learning rate for laparoscopic surgical skills on MIST VR, a virtual reality simulator: quality of human-computer interface. Ann R Coll Surg 81:281–286
Schijven MP, Klaassen R, Jakimowicz J, Terpstra OT (2003) The intercollegiate basic surgical skills course. Surg Endosc 17:1978–1984
Woodrum D, Andreatta P, Yellamanchilla R, Feryus L, Gauger P, Minter R (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191:28–32
McNatt S, Smith CD (2001) A computer-based laparoscopic skills assessment device differentiates experienced from novice laparoscopic surgeons. Surg Endosc 15:1085–1089
Datta V, Chang A, Mackay S, Darzi A (2002) The relationship between motion analysis and surgical technical assessments. Am J Surg 184:70–73
Scott DJ, Rege RV, Bergen PC, Guo WA, Laycock R, Tesfay ST, Valentine RJ, Jones DB (2000) Measuring operative performance after laparoscopic skills training: edited videotape versus direct observation. J LaparoendoscAdv Surg Tech 10:183–190
Thomas W (2006) Teaching and assessing surgical competence. Ann R Coll Surg 88:429–432
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pellen, M.G.C., Horgan, L.F., Barton, J.R. et al. Construct validity of the ProMIS laparoscopic simulator. Surg Endosc 23, 130–139 (2009). https://doi.org/10.1007/s00464-008-0066-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0066-y