Abstract
Backgrounds
Recently, the endoscopic surgical skills of surgeons have become a focus of many investigators and society as a whole. Hence, the importance of the training and education programs used to ensure safer endoscopic surgery has been gradually increasing. We developed our own motion analysis system called the HUESAD, and already demonstrated its construct validity. In this study, we verified that another motion analysis system (which uses the Dartfish Software program) could assess surgeons’ endoscopic surgical skills.
Methods
Experts (who had performed more than 100 laparoscopic surgeries) and novices (who had no experience performing laparoscopic surgery) were recruited for this study. The task was suturing in a dry box trainer. The time and the locus tracing of both sides’ needle holders were analyzed using the new video analysis system (Dartfish Software).
Results
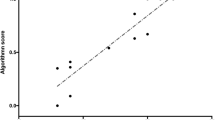
There were statistically significant differences between the experts and novices in all three variables assessed (task time: p = 0.0011, the locus tracing of the left sides’ needle holders: p = 0.0011, the locus tracing of the right sides’ needle holders: p = 0.0011).
Conclusions
The results of this study demonstrated that the results of the motion analysis by the Dartfish Software were well correlated with the surgeon’s skill level.



Similar content being viewed by others
References
Litynski GS (1999) Profiles in laparoscopy: Mouret, Dubois, and Perissat: the laparoscopic breakthrough in Europe (1987–1988). JSLS 3(2):163–167
Botden SM, Buzink SN, Schijven MP, Jakimowicz JJ (2007) Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg 31(4):764–772. doi:10.1007/s00268-006-0724-y
Guidelines for granting of privileges for laparoscopic and/or thoracoscopic general surgery. Society of American Gastrointestinal Endoscopic Surgeons (SAGES) (1998). Surg Endosc 12(4):379–380
Training and assessment of competence (1994). Surg Endosc 8(6):721–722
Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, Brown M (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84(2):273–278
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, Hutchison C (1999) Assessment of technical skills transfer from the bench training model to the human model. Am J Surg 177(2):167–170
Gallagher AG, Lederman AB, McGlade K, Satava RM, Smith CD (2004) Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) using criteria levels based on expert performance. Surg Endosc 18(4):660–665. doi:10.1007/s00464-003-8176-z
Maithel S, Sierra R, Korndorffer J, Neumann P, Dawson S, Callery M, Jones D, Scott D (2006) Construct and face validity of MIST-VR, Endotower, and CELTS: are we ready for skills assessment using simulators? Surg Endosc 20(1):104–112. doi:10.1007/s00464-005-0054-4
Zhang A, Hunerbein M, Dai Y, Schlag PM, Beller S (2008) Construct validity testing of a laparoscopic surgery simulator (Lap Mentor): evaluation of surgical skill with a virtual laparoscopic training simulator. Surg Endosc 22(6):1440–1444. doi:10.1007/s00464-007-9625-x
Yamaguchi S, Konishi K, Yasunaga T, Yoshida D, Kinjo N, Kobayashi K, Ieiri S, Okazaki K, Nakashima H, Tanoue K, Maehara Y, Hashizume M (2007) Construct validity for eye-hand coordination skill on a virtual reality laparoscopic surgical simulator. Surg Endosc 21(12):2253–2257. doi:10.1007/s00464-007-9362-1
Duffy AJ, Hogle NJ, McCarthy H, Lew JI, Egan A, Christos P, Fowler DL (2005) Construct validity for the LAPSIM laparoscopic surgical simulator. Surg Endosc 19(3):401–405. doi:10.1007/s00464-004-8202-9
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191(1):28–32. doi:10.1016/j.amjsurg.2005.10.018
Pellen MG, Horgan LF, Barton JR, Attwood SE (2009) Construct validity of the ProMIS laparoscopic simulator. Surg Endosc 23(1):130–139. doi:10.1007/s00464-008-0066-y
Datta V, Mandalia M, Mackay S, Chang A, Cheshire N, Darzi A (2002) Relationship between skill and outcome in the laboratory-based model. Surgery 131(3):318–323
Bann SD, Khan MS, Darzi AW (2003) Measurement of surgical dexterity using motion analysis of simple bench tasks. World J Surg 27(4):390–394. doi:10.1007/s00268-002-6769-7
Moorthy K, Munz Y, Dosis A, Bello F, Chang A, Darzi A (2004) Bimodal assessment of laparoscopic suturing skills: construct and concurrent validity. Surg Endosc 18(11):1608–1612. doi:10.1007/s00464-003-9312-5
Francis NK, Hanna GB, Cuschieri A (2002) The performance of master surgeons on the Advanced Dundee Endoscopic Psychomotor Tester: contrast validity study. Arch Surg 137(7):841–844
Macmillan AI, Cuschieri A (1999) Assessment of innate ability and skills for endoscopic manipulations by the Advanced Dundee Endoscopic Psychomotor Tester: predictive and concurrent validity. Am J Surg 177(3):274–277
Egi H, Okajima M, Yoshimitsu M, Ikeda S, Miyata Y, Masugami H, Kawahara T, Kurita Y, Kaneko M, Asahara T (2008) Objective assessment of endoscopic surgical skills by analyzing direction-dependent dexterity using the Hiroshima University Endoscopic Surgical Assessment Device (HUESAD). Surg Today 38(8):705–710. doi:10.1007/s00595-007-3696-0
Egi H, Tokunaga M, Hattori M, Ohdan H (2012) Evaluating the correlation between the HUESAD and OSATS scores: concurrent validity study. Minim Invasive Ther Allied Technol. doi:10.3109/13645706.2012.742113
Egi H, Okajima M, Kawahara T, Yoshimitsu M, Sumitani D, Tokunaga M, Takeda H, Itamoto T, Ohdan H (2010) Scientific assessment of endoscopic surgical skills. Minim Invasive Ther Allied Technol 19(1):30–34. doi:10.3109/13645700903493017
Tokunaga M, Egi H, Hattori M, Yoshimitsu M, Sumitani D, Kawahara T, Okajima M, Ohdan H (2012) Approaching time is important for assessment of endoscopic surgical skills. Minim Invasive Ther Allied Technol. doi:10.3109/13645706.2011.596547
Rucci JA, Tomporowski PD (2010) Three types of kinematic feedback and the execution of the hang power clean. J Strength Cond Res 24(3):771–778. doi:10.1519/JSC.0b013e3181cbab96
Xafis V, Babidge W, Field J, Altree M, Marlow N, Maddern G (2013) The efficacy of laparoscopic skills training in a mobile simulation unit compared with a fixed site: a comparative study. Surg Endosc. doi:10.1007/s00464-013-2798-6
Padulo J, Annino G, Migliaccio GM, D’Ottavio S, Tihanyi J (2012) Kinematics of running at different slopes and speeds. J Strength Cond Res 26(5):1331–1339. doi:10.1519/JSC.0b013e318231aafa
Mason JD, Ansell J, Warren N, Torkington J (2013) Is motion analysis a valid tool for assessing laparoscopic skill? Surg Endosc 27(5):1468–1477. doi:10.1007/s00464-012-2631-7
Tokunaga M, Okajima M, Egi H, Yoshimitsu M, Sumitani D, Kawahara T, Hattori M, Ohdan H (2010) The importance of stressing the use of laparoscopic instruments in the initial training for laparoscopic surgery using box trainers: a Randomized Control Study. J Surg Res. doi:10.1016/j.jss.2010.11.906
Panait L, Akkary E, Bell RL, Roberts KE, Dudrick SJ, Duffy AJ (2009) The role of haptic feedback in laparoscopic simulation training. J Surg Res 156(2):312–316. doi:10.1016/j.jss.2009.04.018
Disclosures
Drs. Takashi Suzuki, Hiroyuki Egi, Minoru Hattori, Masakazu Tokunaga, Hiroyuki Sawada and Hideki Ohdan have no competing interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, T., Egi, H., Hattori, M. et al. An evaluation of the endoscopic surgical skills assessment using a video analysis software program. Surg Endosc 29, 1804–1808 (2015). https://doi.org/10.1007/s00464-014-3863-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3863-5