Abstract
Objective
Reconstruction of large and complex bone segments is a challenging problem facing maxillofacial surgery. The majority of current regenerative approaches rely on extrinsic vascularization, which is deficient after cancer ablation and irradiation. The aim of the study was to investigate the efficacy of intrinsic axial vascularization of synthetic bone scaffolds in the management of critical-size mandibular defects.
Materials and methods
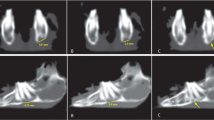
Scaffold-guided mandibular regeneration in two groups of adult male goats was compared. Only the scaffolds of the second group were axially vascularized via in situ embedding of an arteriovenous loop through microsurgical anastomosis of facial vessels. After 6 months of follow up, both groups were compared through radiological, biomechanical, histological and histomorphometric analysis.
Results
The axially vascularized constructs have showed significantly more central vascularization (p = 0.021) and markedly enhanced central bone formation (p = 0.08). The biomechanical characteristics were enhanced, but the difference between both groups was not statistically significant (p = 0.98).
Conclusions
Axially vascularized synthetic mandibular grafts show better vascularization at their central regions, permitting more efficient bone regeneration.
Clinical relevance
The encouraging results of the proposed technique could be of benefit in optimizing the reconstruction of large critical-size bone defects.





Similar content being viewed by others
References
Horch RE, Kneser U, Polykandriotis E, Schmidt VJ, Sun J, Arkudas A (2012) Tissue engineering and regenerative medicine—where do we stand? J Cell Mol Med 16(6):1157–1165. doi:10.1111/j.1582-4934.2012.01564.x
Rath SN, Strobel LA, Arkudas A, Beier JP, Maier AK, Greil P, Horch RE, Kneser U (2012) Osteoinduction and survival of osteoblasts and bone-marrow stromal cells in 3D biphasic calcium phosphate scaffolds under static and dynamic culture conditions. J Cell Mol Med 16(10):2350–2361. doi:10.1111/j.1582-4934.2012.01545.x
Fricain JC, Schlaubitz S, Le Visage C, Arnault I, Derkaoui SM, Siadous R, Catros S, Lalande C, Bareille R, Renard M, Fabre T, Cornet S, Durand M, Leonard A, Sahraoui N, Letourneur D, Amedee J (2013) A nano-hydroxyapatite–pullulan/dextran polysaccharide composite macroporous material for bone tissue engineering. Biomaterials 34(12):2947–2959. doi:10.1016/j.biomaterials.2013.01.049
Hodde J (2002) Naturally occurring scaffolds for soft tissue repair and regeneration. Tissue Eng 8(2):295–308. doi:10.1089/107632702753725058
Pellegrini G, Seol YJ, Gruber R, Giannobile WV (2009) Pre-clinical models for oral and periodontal reconstructive therapies. J Dent Res 88(12):1065–1076. doi:10.1177/0022034509349748
Schliephake H (2013) Clinical efficacy of growth factors to enhance tissue repair in oral and maxillofacial reconstruction: a systematic review. Clin Implant Dent Relat Res. doi:10.1111/cid.12114
Freed LE, Guilak F, Guo XE, Gray ML, Tranquillo R, Holmes JW, Radisic M, Sefton MV, Kaplan D, Vunjak-Novakovic G (2006) Advanced tools for tissue engineering: scaffolds, bioreactors, and signaling. Tissue Eng 12(12):3285–3305. doi:10.1089/ten.2006.12.3285
Kaully T, Kaufman-Francis K, Lesman A, Levenberg S (2009) Vascularization—the conduit to viable engineered tissues. Tissue Eng B Rev 15(2):159–169. doi:10.1089/ten.teb.2008.0193
Kneser U, Polykandriotis E, Ohnolz J, Heidner K, Grabinger L, Euler S, Amann KU, Hess A, Brune K, Greil P, Sturzl M, Horch RE (2006) Engineering of vascularized transplantable bone tissues: induction of axial vascularization in an osteoconductive matrix using an arteriovenous loop. Tissue Eng 12(7):1721–1731. doi:10.1089/ten.2006.12.1721
Polykandriotis E, Arkudas A, Horch RE, Sturzl M, Kneser U (2007) Autonomously vascularized cellular constructs in tissue engineering: opening a new perspective for biomedical science. J Cell Mol Med 11(1):6–20. doi:10.1111/j.1582-4934.2007.00012.x
Morrison WA, Dvir E, Doi K, Hurley JV, Hickey MJ, O'Brien BM (1990) Prefabrication of thin transferable axial-pattern skin flaps: an experimental study in rabbits. Br J Plast Surg 43(6):645–654
Guo L, Pribaz JJ (2009) Clinical flap prefabrication. Plast Reconstr Surg 124(6 Suppl):e340–e350. doi:10.1097/PRS.0b013e3181bcf094
Erol OO, Spira M (1979) New capillary bed formation with a surgically constructed arteriovenous fistula. Surg Forum 30:530–531
Kneser U, Schaefer DJ, Polykandriotis E, Horch RE (2006) Tissue engineering of bone: the reconstructive surgeon's point of view. J Cell Mol Med 10(1):7–19
Eweida AM, Nabawi AS, Marei MK, Khalil MR, Elhammady HA (2011) Mandibular reconstruction using an axially vascularized tissue-engineered construct. Ann Surg Innov Res 5:2. doi:10.1186/1750-1164-5-2
Eweida AM, Nabawi AS, Elhammady HA, Marei MK, Khalil MR, Shawky MS, Arkudas A, Beier JP, Unglaub F, Kneser U, Horch RE (2012) Axially vascularized bone substitutes: a systematic review of literature and presentation of a novel model. Arch Orthop Trauma Surg 132(9):1353–1362. doi:10.1007/s00402-012-1550-3
Beier JP, Horch RE, Arkudas A, Polykandriotis E, Bleiziffer O, Adamek E, Hess A, Kneser U (2009) De novo generation of axially vascularized tissue in a large animal model. Microsurgery 29(1):42–51. doi:10.1002/micr.20564
Beier JP, Horch RE, Hess A, Arkudas A, Heinrich J, Loew J, Gulle H, Polykandriotis E, Bleiziffer O, Kneser U (2010) Axial vascularization of a large volume calcium phosphate ceramic bone substitute in the sheep AV loop model. J Tissue Eng Regen Med 4(3):216–223. doi:10.1002/term.229
Lopez-Heredia MA, Bongio M, Cuijpers VM, van Dijk NW, van den Beucken JJ, Wolke JG, Jansen JA (2012) Bone formation analysis: effect of quantification procedures on the study outcome. Tissue Eng C Methods 18(5):369–373. doi:10.1089/ten.TEC.2011.0353
Yazar S (2007) Selection of recipient vessels in microsurgical free tissue reconstruction of head and neck defects. Microsurgery 27(7):588–594. doi:10.1002/micr.20407
Arkudas A, Balzer A, Buehrer G, Arnold I, Hoppe A, Detsch R, Newby P, Fey T, Greil P, Horch RE, Boccaccini AR, Kneser U (2013) Evaluation of angiogenesis of bioactive glass in the arteriovenous loop model. Tissue Eng C Methods 19(6):479–486. doi:10.1089/ten.TEC.2012.0572
Lokmic Z, Mitchell GM (2008) Engineering the microcirculation. Tissue Eng B Rev 14(1):87–103. doi:10.1089/teb.2007.0299
Cassell OC, Hofer SO, Morrison WA, Knight KR (2002) Vascularisation of tissue-engineered grafts: the regulation of angiogenesis in reconstructive surgery and in disease states. Br J Plast Surg 55(8):603–610
Zhang N, Mustin D, Reardon W, Almeida AD, Mozdziak P, Mrug M, Eisenberg LM, Sedmera D (2006) Blood-borne stem cells differentiate into vascular and cardiac lineages during normal development. Stem Cells Dev 15(1):17–28. doi:10.1089/scd.2006.15.17
Williams SH, Vinyard CJ, Wall CE, Hylander WL (2009) Mandibular corpus bone strain in goats and alpacas: implications for understanding the biomechanics of mandibular form in selenodont artiodactyls. J Anat 214(1):65–78. doi:10.1111/j.1469-7580.2008.01008.x
Ross CF, Dharia R, Herring SW, Hylander WL, Liu ZJ, Rafferty KL, Ravosa MJ, Williams SH (2007) Modulation of mandibular loading and bite force in mammals during mastication. J Exp Biol 210(Pt 6):1046–1063. doi:10.1242/jeb.02733
Vaccaro AR (2002) The role of the osteoconductive scaffold in synthetic bone graft. Orthopedics 25(5 Suppl):s571–s578
Fleming JE Jr, Cornell CN, Muschler GF (2000) Bone cells and matrices in orthopedic tissue engineering. Orthop Clin North Am 31(3):357–374
Raida M, Heymann AC, Gunther C, Niederwieser D (2006) Role of bone morphogenetic protein 2 in the crosstalk between endothelial progenitor cells and mesenchymal stem cells. Int J Mol Med 18(4):735–739
Hu ZM, Peel SA, Ho SK, Sandor GK, Clokie CM (2009) Comparison of platelet-rich plasma, bovine BMP, and rhBMP-4 on bone matrix protein expression in vitro. Growth Factors 27(5):280–288. doi:10.1080/08977190903137819
Park EJ, Kim ES, Weber HP, Wright RF, Mooney DJ (2008) Improved bone healing by angiogenic factor-enriched platelet-rich plasma and its synergistic enhancement by bone morphogenetic protein-2. Int J Oral Maxillofac Implants 23(5):818–826
Malhotra A, Pelletier MH, Yu Y, Walsh WR (2013) Can platelet-rich plasma (PRP) improve bone healing? A comparison between the theory and experimental outcomes. Arch Orthop Trauma Surg 133(2):153–165. doi:10.1007/s00402-012-1641-1
Schuckert KH, Jopp S, Osadnik M (2010) Modern bone regeneration instead of bone transplantation: a combination of recombinant human bone morphogenetic protein-2 and platelet-rich plasma for the vertical augmentation of the maxillary bone-a single case report. Tissue Eng C Methods 16(6):1335–1346. doi:10.1089/ten.TEC.2010.0020
Elshahat A (2006) Correction of craniofacial skeleton contour defects using bioactive glass particles. Egypt J Plast Reconstr Surg 30:113
Clokie CM, Sandor GK (2008) Reconstruction of 10 major mandibular defects using bioimplants containing BMP-7. J Can Dent Assoc 74(1):67–72
Trautvetter W, Kaps C, Schmelzeisen R, Sauerbier S, Sittinger M (2011) Tissue-engineered polymer-based periosteal bone grafts for maxillary sinus augmentation: five-year clinical results. J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 69(11):2753–2762. doi:10.1016/j.joms.2011.02.096
Schuckert KH, Jopp S, Teoh SH (2009) Mandibular defect reconstruction using three-dimensional polycaprolactone scaffold in combination with platelet-rich plasma and recombinant human bone morphogenetic protein-2: de novo synthesis of bone in a single case. Tissue Eng Part A 15(3):493–499. doi:10.1089/ten.tea.2008.0033
Acknowledgments
The authors would like to acknowledge Mrs. Arnold, Mr. Fleischer and Mrs. Weigand for their valuable technical assistance. Some results were presented in the doctoral thesis of Dr. Eweida. The study was funded by a research grant from Alexandria University (AlexREP).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eweida, A.M., Nabawi, A.S., Abouarab, M. et al. Enhancing mandibular bone regeneration and perfusion via axial vascularization of scaffolds. Clin Oral Invest 18, 1671–1678 (2014). https://doi.org/10.1007/s00784-013-1143-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1143-8