Abstract
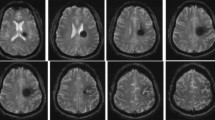
Surgical access to deep intracranial lesions causing the least amount of iatrogenic trauma to the surrounding brain tissue remains a challenging task. In this article, we evaluate the use of a set of sequential tubes that dilate and provide retraction of the overlying brain tissue acting as a surgical corridor for deep-seated brain lesions resection. In addition, we conducted a comprehensive review of the literature of previously described techniques using variable brain tubular retractor systems. We discuss the adaptation of a system designed for spinal use to intracranial pathologies and evaluate the outcomes for the patients involved in the study. Moreover, the advantages and limitations of the described technique were presented. Between August 2005 and 2011, a total of 30 patients with deep brain lesions were operated on using an incremental increase of tubing size for brain retraction guided by a frameless navigation device. Of these, seven cases were intraventricular, and 23 were intraparenchymal. Gross total resection was achieved in 70 % of cases, and the remaining had planned subtotal resections due to involvement of an eloquent area. In conclusion, the technique of serial dilatation of the brain tissue can be used in conjunction with a microscope or endoscope to provide satisfactory access to deep intracranial pathologies. It appears to minimize the associated retraction injury to the surrounding tissue by gradually dilating the white fiber tracts. This operative approach may be considered as an effective and safe alternative for brain tumor resections in selected cases, especially deep-seated lesions.




Similar content being viewed by others
References
Akai T, Shiraga S, Sasagawa Y, Okamoto K, Tachibana O, Lizuka H (2008) Intra-parenchymal tumor biopsy using neuroendoscopy with navigation. Minim Invasive Neurosurg 51(2):83–86
Andrews RJ, Bringas JR (1993) A review of brain retraction and recommendations for minimizing intraoperative brain injury. Neurosurgery 33(6):1052–1063
Bakshi A, Bakshi A, Banerji AK (2004) Neuroendoscope-assisted evacuation of large intracerebral hematomas: introduction of a new, minimally invasive technique. Preliminary report. Neurosurg Focus 16(6):E9
Barlas O, Karadereler S (2004) Stereotactically guided microsurgical removal of colloid cysts. Acta Neurochir (Wien) 146(11):1199–1204
Cabbell KL, Ross DA (1996) Stereotactic microsurgical craniotomy for the treatment of third ventricular colloid cysts. Neurosurgery 38(2):301–307
Chen CC, Cho DY, Chang CS, Chen JT, Lee WY, Lee HC (2005) A stainless steel sheath for endoscopic surgery and its application in surgical evacuation of putaminal haemorrhage. J Clin Neurosci 12(8):937–940
Cohen-Gadol AA (2011) Minitubular transcortical microsurgical approach for gross total resection of third ventricular colloid cysts: technique and assessment. World Neurosurg. Available via DIALOG. http://www.ScienceDirect.com. Accessed 14 Feb 2012
Dujovny M, Ibe O, Perlin A, Ryder T (2010) Brain retractor systems. Neurol Res 32(7):675–83
Engh JA, Lunsford LD, Amin DV, Ochalski PG, Fernandez-Miranda J, Prevedello DM, Kassam AB (2010) Stereotactically guided endoscopic port surgery for intraventricular tumor and colloid cyst resection. Neurosurgery 67(3):S198–S204
Fahim DK, Relyea K, Nayar VV, Fox BD, Whitehead WE, Curry DJ, Luerssen TG, Jea A (2009) Transtubular microendoscopic approach for resection of a choroidal arteriovenous malformation. J Neurosurg Pediatr 3(2):101–104
Fernandez-Miranda JC, Engh JA, Pathak SK, Madhok R, Boada FE, Schneider W, Kassam AB (2010) High-definition fiber tracking guidance for intraparenchymal endoscopic port surgery. J Neurosurg 113(5):990–999
Foley KT, Smith MM, Rampersaud YR (1999) Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus 7(5):E5
Fong S, DuPlessis S (2005) Minimally invasive lateral mass plating in the treatment of posterior cervical trauma: surgical technique. J Spinal Disord Tech 18(3):224–228
Fong S, DuPlessis SJ (2005) Minimally invasive anterior approach to upper cervical spine: surgical technique. J Spinal Disord Tech 18(4):321–325
Greenberg IM (1981) Self-retaining retractor and handrest system for neurosurgery. Neurosurgery 8(2):205–208
Greenfield JP, Cobb WS, Tsouris AJ, Schwartz TH (2008) Stereotactic minimally invasive tubular retractor system for deep brain lesions. Neurosurgery 63(4 Suppl 2):334–339
Haji FA, Cenic A, Crevier L, Murty N, Reddy K (2011) Minimally invasive approach for the resection of spinal neoplasm. Spine (Phila, Pa 1976) 36(15):E1018–1026
Harris AE, Hadjipanayis CG, Lunsford LD, Lunsford AK, Kassam AB (2005) Microsurgical removal of intraventricular lesions using endoscopic visualization and stereotactic guidance. Neurosurgery 56(1):125–132
Herrera SR, Shin JH, Chan M, Kouloumberis P, Goellner E, Slavin KV (2010) Use of transparent plastic tubular retractor in surgery for deep brain lesions: a case series. Surg Technol Int 19:47–50
Ichinose T, Goto T, Morisako H, Takami T, Ohata K (2010) Microroll retractor for surgical resection of brainstem cavernomas. World Neurosurg 73(5):520–522
Ishii K, Matsumoto M, Watanabe K, Nakamura M, Chiba K, Toyama Y (2005) Endoscopic resection of cystic lesions in the lumbar spinal canal: a report of two cases. Minim Invasive Neurosurg 48(4):240–243
Jho HD, Alfieri A (2002) Endoscopic removal of third ventricular tumors: a technical note. Minim Invasive Neurosurg 45(2):114–119
Jo KI, Chung SB, Jo KW, Kong DS, Seol HJ, Shin HJ (2011) Microsurgical resection of deep-seated lesions using transparent tubular retractor: pediatric case series. Childs Nerv Syst 27(11):1989–1994
Jo KW, Shin HJ, Nam DH, Lee JI, Park K, Kim JH, Kong DS (2011) Efficacy of endoport-guided endoscopic resection for deep-seated brain lesions. Neurosurg Rev 34(4):457–463
Kassam AB, Engh JA, Mintz AH, Prevedello DM (2009) Completely endoscopic resection of intraparenchymal brain tumors. J Neurosurg 110(1):116–123
Kelly PJ (1989) Future perspectives in stereotactic neurosurgery: stereotactic microsurgical removal of deep brain tumors. J Neurosurg Sci 33(1):149–154
Kelly PJ, Alker GJ Jr (1981) A stereotactic approach to deep-seated central nervous system neoplasms using the carbon dioxide laser. Surg Neurol 15(5):331–334
Kelly PJ, Goerss SJ, Kall BA (1988) The stereotaxic retractor in computer-assisted stereotaxic microsurgery. Technical note. J Neurosurg 69(2):301–306
Kelly PJ, Kall BA, Goerss S, Earnest F 4th (1986) Computer-assisted stereotaxic laser resection of intra-axial brain neoplasms. J Neurosurg 64(3):427–439
Kelly PJ, Kall BA, Goerss SJ (1987) Computer-interactive stereotactic resection of deep-seated and centrally located intraaxial brain lesions. Appl Neurophysiol 50(1–6):107–113
Khoo LT, Palmer S, Laich DT, Fessler RG (2002) Minimally invasive percutaneous posterior lumbar interbody fusion. Neurosurgery 51(5):S166–171
Kim DH, O’Toole JE, Ogden AT, Eichholz KM, Song J, Christie SD, Fessler RG (2009) Minimally invasive posterolateral thoracic corpectomy: cadaveric feasibility study and report of four clinical cases. Neurosurgery 64(4):746–752
Kurimoto M, Hayashi N, Kamiyama H, Nagai S, Shibata T, Asahi T, Matsumura N, Hirashima Y, Endo S (2004) Impact of neuronavigation and image-guided extensive resection for adult patients with supratentorial malignant astrocytomas: a single-institution retrospective study. Minim Invasive Neurosurg 47(5):278–283
McLaughlin N, Prevedello DM, Engh J, Kelly DF, Kassam AB (2012) Endoneurosurgical resection of intraventricular and intraparenchymal lesions using the port technique. World Neurosurg. Available via DIALOG. http://www.ScienceDirect.com. Accessed 18 Mar 2012
Melamed I, Merkin V, Korn A, Nash M (2005) The supraorbital approach: an alternative to traditional exposure for the surgical management of anterior fossa and parasellar pathology. Minim Invasive Neurosurg 48(5):259–263
Moshel YA, Link MJ, Kelly PJ (2007) Stereotactic volumetric resection of thalamic pilocytic astrocytomas. Neurosurgery 61(1):66–75
Nakano T, Ohkuma H, Asano K, Ogasawara Y (2007) Endoscopic treatment for deep-seated or multiple intraparenchymal tumors: technical note. Minim Invasive Neurosurg 52(1):59–52
Nishihara T, Nagata K, Tanaka S, Suzuki Y, Izumi M, Mochizuki Y, Akabane A, Ochiai C (2005) Newly developed endoscopic instruments for the removal of intracerebral hematoma. Neurocrit Care 2(1):67–74
Nishihara T, Teraoka A, Morita A, Ueki K, Takai K, Kirino T (2000) A transparent sheath for endoscopic surgery and its application in surgical evacuation of spontaneous intracerebral hematomas. Technical note. J Neurosurg 92(6):1053–1055
Ogura K, Tachibana E, Aoshima C, Sumitomo M (2006) New microsurgical technique for intraparenchymal lesions of the brain: transcylinder approach. Acta Neurochir (Wien) 148(7):779–785
Otsuki T, Jokura H, Yoshimoto T (1990) Stereotactic guiding tube for open-system endoscopy: a new approach for the stereotactic endoscopic resection of intra-axial brain tumors. Neurosurgery 27(2):326–330
Palmer S (2002) Use of a tubular retractor system in microscopic lumbar discectomy: 1 year prospective results in 135 patients. Neurosurg Focus 13(2):E5
Palmer S, Turner R, Palmer R (2002) Bilateral decompressive surgery in lumbar spinal stenosis associated with spondylolisthesis: unilateral approach and use of a microscope and tubular retractor system. Neurosurg Focus 13(1):E4
Patil AA (1987) Stereotactic excision of deep brain lesions using probe guided brain retractor. Acta Neurochir (Wien) 87(3–4):150–152
Raza SM, Recinos PF, Avendano J, Adams H, Jallo GI, Quinones-Hinojosa A (2011) Minimally invasive trans-portal resection of deep intracranial lesions. Minim Invasive Neurosurg 54(1):5–11
Recinos PF, Raza SM, Jallo GI, Recinos VR (2011) Use of a minimally invasive tubular retraction system for deep-seated tumors in pediatric patients. J Neurosurg Pediatr 7(5):516–521
Ross DA (1993) A simple stereotactic retractor for use with the Leksell stereotactic system. Neurosurgery 32(3):475–476
Singh L, Agrawal N (2009) Cylindrical channel retractor for intraventricular tumour surgery—a simple and inexpensive device. Acta Neurochir (Wien) 151(11):1493–7
Sugita K, Hirota T, Mizutani T, Mutsuga N, Shibuya M, Tsugane R (1978) A newly designed multipurpose microneurosurgical head frame. Technical note. J Neurosurg 48(4):656–657
Tan TC, McL Black P (2003) Image-guided craniotomy for cerebral metastases: techniques and outcomes. Neurosurgery 53(1):82–89
Vasudevan RR, Galvan G, Pait GT, Villavicenico AT, Bulsara KR (2007) Muscle splitting approach with MetrX system for removal of intrathecal bullet fragment: a case report. J Trauma 62(5):1290–1291
Wadley J, Dorward N, Kitchen N, Thomas D (1999) Pre-operative planning and intra-operative guidance in modern neurosurgery: a review of 300 cases. Ann R Coll Surg Engl 81(4):217–225
Waran V, Vairavan N, Sia SF, Abdullah B (2009) A new expandable cannula system for endoscopic evacuation of intraparenchymal hemorrhages. J Neurosurg 111(6):1127–1130
Yadav YR, Yadav S, Sherekar S, Parihar V (2011) A new minimally invasive tubular brain retractor system for surgery of deep intracerebral hematoma. Neurol India 59(1):74–77
Yasargil MG, Fox JL (1974) The microsurgical approach to acoustic neurinomas. Surg Neurol 2(6):393–398
Zhong J, Dujovny M, Perlin AR, Perez-Arjona E, Park HK, Diaz FG (2003) Brain retraction injury. Neurol Res 25(8):831–838
Conflict of interest
None of the authors have any conflicts of interest. Amin Kassam is a consultant for Karl Storz Endoscopy and Stryker, and has equity interest in the NICO Corporation. The authors have no personal financial or institutional interest in any of the materials or devices described in this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Richard Lochhead, Phoenix, USA
Almenawer et al. present an article entitled "Minimal access to deep intracranial lesions using a serial dilation technique: case-series and review of brain tubular retractor systems." In this article, the authors describe their experience using tubular retractors as a minimally invasive approach to deep cerebral lesions. This tubular retractor equipment is commonly used in the spine and is readily available in many neurosurgical centers. The article includes step-by-step illustrations, experience with 30 cases, selected case examples, and a thorough literature review. The authors should be commended for their work.
Vikram C. Prabhu, Christopher M. Loftus, Maywood, USA
Compared to brain blade retractors, tubular retractors distribute external pressure evenly over a larger area, potentially minimizing cortical injury. They provide a relatively fixed amount of retraction and tamponade adjacent cortex. Intuitively, their use for focal brain lesion surgery seems like a good idea. Almenawer et al. describe their experience with a commercially available tubular retractor system, originally designed for spinal surgery, to resect intracranial tumors in 30 patients over a 6-year span. They used serial dilatation rather than the single-entry technique previously described and purport that it decreases injury to white matter tracts. That is hypothetical; there is no radiographic or clinical evidence to validate it. Other groups have reported similar success using slightly different iterations of the same concept. For intraventricular or subcortical (thalamus and basal ganglia) lesions, or intracerebral hematoma evacuation, the fixed surgical path provided by these systems is ideal and may reduce inaccuracies of the navigation system by minimizing the confounding effect of brain shift. On the other hand, when resecting relatively superficial cortical lesions within 2–3 cm of the pial surface, they may be obtrusive. There are other limitations. The added steps to insert the tube may be cumbersome and the overpass technique described here, unwieldy. The complex three-dimensional morphology of an intra-axial brain tumor requires constant adjustment of the surgical angle and protection or coagulation of adjacent blood vessels. Adjusting the trajectory of these opaque rigid tubes may inadvertently inflict injury on adjacent cortex and white matter and they may constrain dexterity required for intracranial surgery. The venous structures intimately associated with posterior fossa and pineal lesions require careful consideration and may be at risk with a tubular retractor, despite the excellent results demonstrated here.
It is fundamental practice to select the shortest trajectory to a cortical or subcortical lesion that avoids eloquent cortex or essential white matter tracts using intraoperative neuronavigation, or in some centers, intraoperative magnetic resonance image (iMRI) guidance. A certain amount of normal tissue sacrifice is inherent in this process, whether one uses a tubular retractor or not, but it is critical to avoid inadvertent injury to adjacent areas not part of the planned surgical tract. Creating a surgical path under direct visualization provides a measure of safety especially when adopting trans-sulcal approaches where cortical vessels are buried in the depths of the sulcus and along the lateral margins of the adjacent gyri. In a non-hydrocephalic child or adult, the outer margin of the ventricle is generally within 5 cm of the pial surface. Hence, the outer margin of most cortical lesions would be within 2–3 cm of the pial surface and is easily reached without having to resort to the use of retractors of any kind. The popularity of self-retaining planar cortical retractors has waned over the past decade largely because surgeons recognize injury they inflict on adjacent cortex. We almost never utilize fixed retractors for intra-axial tumor resections but rather use a handheld Penfield #2 over a soft cotton or telfa patty to gently hold the cortex away and keep the field open — the fatiguing hand of the person holding the Penfield #2 ensures only brief periods of retraction. For trans-sulcal approaches, we gently wedge a cotton-ball in place to keep the surgical path open, a nuance Dr. Yasargil taught. However, the dynamic interface between cortical tissue and a tubular retractor is unique. They may function as restrainers (holding back cortical tissue that would migrate into the surgical path) rather than a retractors (actively pushing cortical tissue away from the surgical path). In the former scenario, the pressure effect is inward and a function of intrinsic brain tissue pressure and pulsatility, while in the latter case, it is an outward pressure and a function of the force applied by the retractor arm (human or mechanical). A slight difference, but important when operating on deep lesions in proximity to essential cortex or white matter tracts such as the internal capsule. And there are other considerations when selecting the optimal tubular retractor system. The commercially available clear plastic ovoid tubes designed for cranial surgery may have a slight advantage over the system used here and would be iMRI compatible. Other adjuncts such as preoperative functional MRI and diffusion tensor imaging data help determine the surgical access point and tract and in some instances, electrophysiological or awake cortical mapping would be ideal modalities to preserve neurological function. In the end, careful case selection based on anatomy and pathology is essential; in some instances, a stereotactic biopsy may be the best course. This is simply a tool that may add a slight advantage to a neurosurgeon’s armamentarium, in select circumstances. It is not a substitute for surgical skill or judgement, and may not determine patient outcome. The authors are commended on their excellent results; it is possible they may have achieved the same through a conventional approach without the use of this retractor.
Guilherme C. Ribas, São Paulo, Brazil
So-called minimal invasive procedures are already very much used with safety and excellent results in the current practice of many surgical specialties, which, unfortunately, is not a reality for the neurosurgery of intrinsic brain lesions yet, despite all efforts and research that has been done in this field as we can appreciate through the extensive list of references of this interesting article. Parallel to the notorious appeal of this concept, the well known difficulties are more particularly related with the compactness of the brain tissue itself, with the dimensions and fragility of the neural and vascular structures, and to the magnitude of potential bleedings (the brain weights approximately 2 % of the body and receives about 10–15 % of the cardiac output!). Even for ventricular and cisternal neurosurgery the currently available technology still allows only very limited surgical interventions.
This article by Almenawer et al. propitiates one step ahead within this issue mostly by describing a clever method of serially dilating an introduced tube through which microsurgical procedures can be then done. Their also reported experience already with 30 actual surgical cases corroborates its feasibility without significant complications. Nevertheless, further optical and instrumental developments are still required for us to operate intrinsic brain lesions through minimally invasive approaches more efficiently and with safety and comfort.
While the improvement of our patients care depends very much on further contribution of other fields, further development of microneurosurgery itself depends on putting together our current knowledge of morphological and functional brain anatomy together with new technology developments, which is achieved mainly through experience and creativity, and this article is definitely pointing to this direction. Further utilization of this technique proposed by Almenawer et al. will evaluate better its use usefulness, and/or will provide contributions for development of new similar techniques.
Rights and permissions
About this article
Cite this article
Almenawer, S.A., Crevier, L., Murty, N. et al. Minimal access to deep intracranial lesions using a serial dilatation technique. Neurosurg Rev 36, 321–330 (2013). https://doi.org/10.1007/s10143-012-0442-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0442-x