Abstract
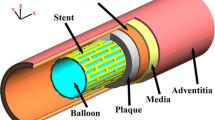
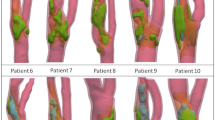
Plaque rupture plays a role in the majority of acute coronary syndromes. Rupture has usually been associated with stress concentrations, which are mainly affected by the plaque geometry and the tissue properties. The aim of this study is to evaluate the influence of morphology on the risk of plaque rupture, including the main geometrical factors, and to assess the role of circumferential and axial residual stresses by means of a parametric 3D finite element model. For this purpose, a 3D parametric finite element model of the coronary artery with eccentric atheroma plaque was developed. Healthy (adventitia and media in areas without atheroma plaque) and diseased (fibrotic and lipidic) tissues were considered in the model. The geometrical parameters used to define and design the idealized coronary plaque anatomy were the lipid core length, the stenosis ratio, the fibrous cap thickness, and the lipid core ratio. Finally, residual stresses in longitudinal and circumferential directions were incorporated into the model to analyse the influence of the important mechanical factors in the vulnerability of the plaque. Viewing the results, we conclude that residual stresses should be considered in the modelling of this kind of problems since they cause a significant alteration of the vulnerable plaque region limits. The obtained results show that the fibrous cap thickness and the lipid core length, in combination with the lipid core width, appear to be the key morphological parameters that play a determinant role in the maximal principal stress (MPS). However, the stenosis ratio is found to not play a significant role in vulnerability related to the MPS. Plaque rupture should therefore be observed as a consequence, not only of the cap thickness, but as a combination of the stenosis ratio, the fibrous cap thickness and the lipid core dimensions.
Similar content being viewed by others
References
Alastrué V et al (2007) Assessing the use of the “opening angle method” to enforce residual stresses in patient-specific arteries. Ann Biomed Eng 35: 1821–1837
Armentano R et al (1995) Effects of hypertension on viscoelasticity of carotid and femoral arteries in humans. Hypertension 26: 48–54
Armentano R et al (2006) An in vitro study of cryopreserved and fresh human arteries: a comparison with ePTFE prostheses and human arteries studied non-invasively in vivo. Cryobiology 52: 17–26
Arroyo LH, Lee RT (1999) Mechanisms of plaque rupture: mechanical and biologic interactions. Cardiovasc Res 41: 369–375
Auer M et al (2006) 3-D reconstruction of tissue components for atherosclerotic human arteries using ex vivo high-resolution MRI. Med Imaging 25: 345–357
Bluestein D et al (2008) Influence of microcalcifications on vulnerable plaque mechanics using FSI modelling. J Biomech 41: 1111–1118
Briley-Saebo KC et al (2007) Magnetic resonance imaging of vulnerable atherosclerotic plaques: current imaging strategies and molecular imaging probes. J Magn Reson Imaging 26: 460–479
Carew TE et al (1968) Compressibility of the arterial wall. Circ Res 23: 61–86
Cheng G et al (1993) Distribution of circumferential stress in ruptured and stable atherosclerotic lesions. A structural analysis with histopathological correlation. Circulation 87: 1179–1187
Chun Y et al (2010) Three-dimensional carotid plaque progression simulation using meshless generalized finite difference method based on multi-year MRI patient-tracking data. Comput Model Eng Sci 57: 51–76
Creane A et al (2010) Finite element modelling of diseased carotid bifurcations generated from in vivo computerised tomographic angiography. Comput Biol Med 40: 419–429
Davies MJ (1996) Stability and instability: two faces of coronary atherosclerosis: the Paul Dudley White lecture 1995. Circulation 94: 2013–2020
Davies MJ et al (1993) Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J 69: 377–381
Douglas AF et al (2011) Extracranial carotid plaque length and parent vessel diameter significantly affect baseline ipsilateral intracranial blood flow. Neurosurgery 69: 114–121
Fayad ZA, Fuster V (2001) Clinical imaging of the high-risk or vulnerable atherosclerotic plaque. Circ Res 89: 305–316
Finet G et al (2004) Biomechanical interaction between cap thickness, lipid core composition and blood pressure in vulnerable coronary plaque: impact on stability or instability. Coron Artery Dis 15: 13–20
Fujii K et al (2005) Association of plaque characterization by intravascular ultrasound virtual histology and arterial remodeling. Am J Cardiol 96: 1476–1483
Fuster V et al (2005) Atherothrombosis and high-risk plaque: part II: approaches by noninvasive computed tomographic/magnetic resonance imaging. J Am Coll Cardiol 46: 1209–1218
Gao H, Long Q (2008) Effects of varied lipid core volume and fibrous cap thickness on stress distribution in carotid arterial plaques. J Biomech 41: 3053–3059
Gasser TC et al (2006) Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J R Soc Interface 3: 15–35
Gertz S, Roberts WC (1990) Hemodynamic shear force in rupture of coronary arterial atherosclerotic plaques. Am J Cardiol 66: 1368–1372
Hanke CFG, Lenz H (2001) The discovery of the pathophysiological aspects of atherosclerosis—a review. Acta Chirurgica Belgica 101: 162–169
Himburg HA et al (2004) Spatial comparison between wall shear stress measures and porcine arterial endothelial permeability. Am J Physiol Heart 286: H1916–H1922
Holzapfel GA et al (2005) Determination of the layer-specific mechanical properties of human coronary arteries with non-atherosclerotic intimal thickening, and related constitutive modelling. Am J Physiol Heart 289: H2048–H2058
Huang H et al (2001) The impact of calcification on the biomechanical stability of atherosclerotic plaques. Circulation 103: 1051–1056
Imoto K et al (2005) Longitudinal structural determinants of atherosclerotic plaque vulnerability: a computational analysis of stress distribution using vessel models and three-dimensional intravascular ultrasound imaging. J Am Coll Cardiol 46: 1507–1515
Jaroslav V et al (1999) Residual strain in human atherosclerotic coronary arteries and age related geometrical changes. Biomed Mater Eng 9: 311–317
Jaroslav V et al (2002) Age related constitutive laws and stress distribution in human main coronary arteries with reference to residual strain. Biomed Mater Eng 12: 121–134
Kips JG et al (2008) Identifying the vulnerable plaque: a review of invasive and non-invasive imaging modalities. Artery Res 2: 21–34
Kock SA et al (2008) Mechanical stresses in carotid plaques using MRI-based fluid-structure interaction models. J Biomech 41: 1651–1658
Krishna Kumar R, Balakrishnan KR (2005) Influence of lumen shape and vessel geometry on plaque stresses: possible role in the increased vulnerability of a remodelled vessel and the shoulder of a plaque. Heart 91: 1459–1465
Kyriacou S et al (1996) Finite element analysis of non-linear orthotropic hyperelastic membranes. Comput Mech 18: 269–278
Lee R (2000) Atherosclerotic lesion mechanisc versus biology. Zeitschrift fur Kardiologie 89: 80–84
Lee R et al (1993) Computational structural analysis based on intravascular ultrasound imaging before in vitro angioplasty: prediction of plaque fracture locations. J Am Coll Cardiol 21: 777–782
Lendon CL et al (1991) Atherosclerotic plaque caps are locally weakened when macrophages density is increased. Atherosclerosis 87: 87–90
Lloyd-Jones D et al (2009) Heart disease and stroke statistics–2009 update: a report from the American heart association statistics committee and stroke statistics subcommittee. Circulation 119: 21–181
Loree H et al (1992) Effects of fibrous cap thickness on peak circumferential stress in model atherosclerotic vessels. Circ Res 71: 850–858
Loree HM et al (1994) Static circumferential tangential modulus of human atherosclerotic tissue. J Biomech 27: 195–204
Marquardt DW (1963) An algorithm for least-squares estimation of nonlinear parameters. SIAM J Appl Math 11: 431–441
Moreno PR et al (2002) Intimomedial interface damage and adventitial inflammation is increased beneath disrupted atherosclerosis in the aorta: implications for plaque vulnerability. Circulation 105: 2504–2511
Naghavi M et al (2003) From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation 108: 1664–1672
Ohayon J et al (2007) Influence of residual stress/strain on the biomechanical stability of vulnerable coronary plaques: potential impact for evaluating the risk of plaque rupture. Am J Physiol Heart 293: H1987–H1996
Ohayon J et al (2008) Necrotic core thickness and positive arterial remodeling index: emergent biomechanical factors for evaluating the risk of plaque rupture. Am J Physiol Heart 295: H717–H727
Ohayon J et al (2005) A three dimensional finite element analysis of stress distribution in a coronary atherosclerotic plaque: in-vivo prediction of plaque rupture location. Biomech Appl Comput Assist Surg 17: 225–241
Ohayon J et al (2001) In-vivo prediction of human coronary plaque rupture location using intravascular and finite element method. Coron Artery Dis 12: 655–663
Pasterkamp G et al (2000) Arterial remodeling in atherosclerosis, restenosis and after alteration of blood flow: potential mechanisms and clinical implications. Cardiovasc Res 45: 843–852
Peña E et al (2010) A constitutive formulation of vascular tissue mechanics including viscoelasticity and softening behaviour. J Biomech 43: 984–989
Peterson SJ, Okamoto RJ (2000) Effect of residual stress and heterogeneity on circumferential stress in the arterial wall. J Biomech Eng 122: 454–456
Raghavan ML et al (2004) Three-dimensional finite element analysis of residual stress in arteries. Ann Biomed Eng 32: 257–263
Salunke NV et al (2001) Compressive stress-relaxation of human atherosclerotic plaque. J Biomed Mater Res Part A 55: 236–241
Smedby O (1998) Geometrical risk factors for atherosclerosis in the femoral artery: a longitudinal angiographic study. Ann Biomed Eng 26: 391–397
Spencer AJM (1971) Theory of invariants. In: Continuum physics. Academic Press, New York, pp 239–253
Tang D et al (2009) Sites of rupture in human atherosclerotic carotid plaques are associated with high structural stresses: an in vivo MRI-based 3D fluid-structure interaction study. Stroke 40: 3258–3263
Tang D et al (2004) Effect of a liqid pool on stress/strain distributions in stenotic arteries: 3D fluid-structure interactions (FSI) models. ASME J Biomech Eng 126: 363–370
Tang D et al (2005) Local maximal stress hypothesis and computational plaque vulnerability index for atherosclerotic plaque assessment. Ann Biomed Eng 33: 1789–1801
Tang T et al (2008) Correlation of carotid atheromatous plaque inflammation with biomechanical stress: utility of USPIO enhanced MR imaging and finite element analysis. Atherosclerosis 196: 879–887
Thubrikar M (2007) Vascular mechanics and pathology. Spinger, Berlin
Vander Wal AC, Becker AE (1999) Atherosclerotic plaque rupture—pathologic basis of plaque stability and instability. Cardiovasc Res 41: 334–344
VanEpps JS, Vorp DA (2007) Mechanopathobiology of atherogenesis: a review. J Surg Res 142: 202–217
Varnava AM et al (2002) Relationship between coronary artery remodeling and plaque vulnerability. Circulation 105: 939–943
Vengrenyuk Y et al (2006) A hypothesis for vulnerable plaque rupture due to stress-induced debonding around cellular microcalcifications in thin fibrous caps. Proc Natl Acad Sci 103: 14678–14683
Versluis A et al (2006) Fatigue and plaque rupture in myocardial infarction. J Biomech 39: 339–347
Virmani R et al (2006) Pathology of the vulnerable plaque. J Am Coll Cardiol 47: C13–18
Virmani R et al (2000) Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 20: 1262–1275
Williamson SD et al (2003) On the sensitivity of wall stresses in diseased arteries to variable material properties. ASME J Biomech Eng 125: 147–155
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
The Below is the Electronic Supplementary Material.
Rights and permissions
About this article
Cite this article
Cilla, M., Peña, E. & Martínez, M.A. 3D computational parametric analysis of eccentric atheroma plaque: influence of axial and circumferential residual stresses. Biomech Model Mechanobiol 11, 1001–1013 (2012). https://doi.org/10.1007/s10237-011-0369-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-011-0369-0