Abstract
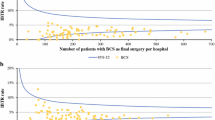
Surgical margin status after first breast-conserving surgery (BCS) is used as a quality indicator of breast cancer care in the Netherlands. The aim is to describe the variation in surgical margin status between hospitals. 7,345 patients with DCIS or invasive cancer (T1-2,N0-1,M0) diagnosed between July 1, 2008, and June 30, 2009, who underwent BCS as first surgery, were selected from the Netherlands Cancer Registry. Patients were treated in 96 hospitals. Maximum target values were 30% ‘focally positive’ or ‘more than focally positive’ for DCIS and 10% ‘more than focally positive’ for invasive carcinoma. Results per hospital are presented in funnel plots. For invasive carcinoma, multivariate logistic regression was used to adjust for case mix. Overall 28.5% (95% CI: 25.5–31.4%) of DCIS and 9.1% (95% CI: 8.4–9.8%) of invasive carcinoma had positive margins. Variation between hospitals was substantial. 6 and 10 hospitals, respectively, for DCIS and invasive cancer showed percentages above the upper limit of agreement. Case mix correction led to significant different conclusions for 5 hospitals. After case mix correction, 10 hospitals showed significant higher rates, while 7 hospitals showed significant lower rates. High rates were not related to breast cancer patient volume or type of hospital (teaching vs. non-teaching). Higher rates were related to hospitals where the policy is to aim for BCS instead of mastectomy. The overall percentage of positive margins in the Netherlands is within the predefined targets. The variation between hospitals is substantial but can be largely explained by coincidence. Case mix correction leads to relevant shifts.



Similar content being viewed by others
References
van Steenbergen LN, van de Poll-Franse LV, Wouters MW, Jansen-Landheer ML, Coebergh JW, Struikmans H et al (2010) Variation in management of early breast cancer in the Netherlands, 2003–2006. Eur J Surg Oncol 36(Suppl 1):S36–S43
National Breast Cancer Organization of the Netherlands. Guideline breast cancer. http://www.oncoline.nl. Accessed 16 June 2011
Het resultaat telt 2008 (2009) The Hague: Dutch health care inspectorate
Gooiker GA, Veerbeek L, van der Geest LG, Stijnen T, Dekker JW, Nortier JW et al (2010) The quality indicator ‘tumour positive surgical margin following breast-conserving surgery’ does not provide transparent insight into care. Ned Tijdschr Geneeskd 154:A1142
Vles WJ (2009) Schone Schijn; Slordige data-interpretatie vloert betrouwbaarheid prestatie-indicator. Medisch Contact 2008(33/34):1354–1356
TNM Classification of Malignant Tumours (2002) 6th edn. UICC, Geneva
Spiegelhalter DJ (2005) Funnel plots for comparing institutional performance. Statist Med 24:1185–1202
Cabioglu N, Hunt KK, Sahin AA, Kuerer HM, Babiera GV, Singletary SE et al (2007) Role for intraoperative margin assessment in patients undergoing breast-conserving surgery. Ann Surg Oncol 14(4):1458–1471
Kurniawan ED, Wong MH, Windle I, Rose A, Mou A, Buchanan M et al (2008) Predictors of surgical margin status in breast-conserving surgery within a breast screening program. Ann Surg Oncol 15(9):2542–2549
Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S et al (2009) The relationship between surgical factors and margin status after breast-conservation surgery for early stage breast cancer. Am J Surg 197(6):740–746
Luini A, Rososchansky J, Gatti G, Zurrida S, Caldarella P, Viale G et al (2009) The surgical margin status after breast-conserving surgery: discussion of an open issue. Breast Cancer Res Treat 113(2):397–402
Dick AW, Sorbero MS, Ahrendt GM, Hayman JA, Gold HT, Schiffhauer L et al (2011)Comparative effectiveness of Ductal carcinoma in situ management and the roles of margins and surgeons. J Natl Cancer Inst 103(2):92–104
Morrow M (2010) Trends in the surgical treatment of breast cancer. Breast J 16(Suppl 1):S17–S19
Azu M, Abrahamse P, Katz SJ, Jagsi R, Morrow M (2010) What is an adequate margin for breast-conserving surgery? Surgeon attitudes and correlates. Ann Surg Oncol 17(2):558–563
Houssami N, Macaskill P, Marinovich ML, Dixon JM, Irwig L, Brennan ME et al (2010) Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur J Cancer 46(18):3219–3232
Kaufmann M, Morrow M, von MG, Harris JR (2010) Locoregional treatment of primary breast cancer: consensus recommendations from an International Expert Panel. Cancer 116(5):1184–1191
Zavagno G, Goldin E, Mencarelli R, Capitanio G, Del BP, Marconato R et al (2008) Role of resection margins in patients treated with breast conservation surgery. Cancer 112(9):1923–1931
Dunne C, Burke JP, Morrow M, Kell MR (2009) Effect of margin status on local recurrence after breast conservation and radiation therapy for ductal carcinoma in situ. J Clin Oncol 27(10):1615–1620
Del Turco MR, Ponti A, Bick U, Biganzoli L, Cserni G, Cutuli B et al (2010) Quality indicators in breast cancer care. Eur J Cancer 46(13):2344–2356
Talsma AK, Reedijk AM, Damhuis RA, Westenend PJ, Vles WJ (2011) Re-resection rates after breast-conserving surgery as a performance indicator: introduction of a case-mix model to allow comparison between Dutch hospitals. Eur J Surg Oncol 37(4):357–363
Virnig BA, Tuttle TM (2011) Random physician effect and comparative effectiveness of treatment for ductal carcinoma in situ. J Natl Cancer Inst 103(2):81–82
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van der Heiden-van der Loo, M., de Munck, L., Visser, O. et al. Variation between hospitals in surgical margins after first breast-conserving surgery in the Netherlands. Breast Cancer Res Treat 131, 691–698 (2012). https://doi.org/10.1007/s10549-011-1809-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1809-3