Abstract
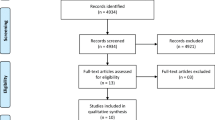
Exercise rehabilitation in heart failure patients has been shown to improve quality of life (QoL) and survival. It is also recommended in clinical practice guidelines for ventricular assist device (VAD) recipients. However, there have only been two meta-analyses on the effects of exercise rehabilitation in VAD patients, on only two outcomes. The objective of the review was to quantitatively evaluate the effect of exercise rehabilitation in VAD recipients on functional capacity, exercise physiology parameters, chronotropic responses, inflammatory biomarkers and neurohormones, heart structure and function, and clinical outcomes. The following databases were systematically searched: CCTR, CDSR, CINAHL, EMBASE, PsycInfo, and Medline through to November 2015, for studies reporting on VAD recipients receiving ≥ 2 sessions of aerobic training. Citations were considered for inclusion, and data were extracted in included studies as well as quality assessed, each by two investigators independently. Random-effects meta-analyses were performed where possible. The meta-analysis showed that compared to usual care, exercise rehabilitation significantly improved peak VO2 (n = 74, mean difference = 1.94 mL kg−1 min−1, 95% CI 0.63–3.26, p = 0.004) and 6-min walk test distance (n = 52, mean difference = 42.46 m, 95% CI 8.45–76.46, p = 0.01). No significant differences were found for the ventilatory equivalent slope (VE/VCO2) or ventilatory anaerobic threshold (VAT). In the six studies which reported QoL, exercise rehabilitation was beneficial in four, with no difference observed in two studies. Exercise rehabilitation is associated with improved outcomes in VAD recipients, and therefore should be more systematically delivered in this population.



Similar content being viewed by others
Abbreviations
- HF:
-
Heart failure
- VADs:
-
Ventricular assist devices
- LVAD:
-
Left ventricular assist device
- QoL:
-
Quality of life
- Peak VO2 :
-
Maximal oxygen consumption (ml/kg/min)
- VE/VCO2 :
-
Ventilatory equivalent
- VAT:
-
Ventilatory anaerobic threshold
References
Mancini D, Goldsmith R, Levin H, Beniaminovitz A, Rose E, Catanese K, Flannery M, Oz M (1998) Comparison of exercise performance in patients with chronic severe heart failure versus left ventricular assist devices. Circulation 98:1178–1183
Jakovljevic DG, George RS, Nunan D, Donovan G, Bougard RS, Yacoub MH, Birks EJ, Brodie DA (2010) The impact of acute reduction of continuous-flow left ventricular assist device support on cardiac and exercise performance. Heart 96:1390–1395
Simon MA, Kormos RL, Gorcsan J 3rd et al (2005) Differential exercise performance on ventricular assist device support. J Heart Lung Transplant 24:1506–1512
Haft J, Armstrong W, Dyke DB et al (2007) Hemodynamic and exercise performance with pulsatile and continuous-flow left ventricular assist devices. Circulation 116:18–15
Leibner ES, Cysyk J, Eleuteri K, el-Banayosy A, Boehmer JP, Pae WE (2013) Changes in the functional status measures of heart failure patients with mechanical assist devices. Am Soc Artif Intern Organs 59:117–122
Grosman-Rimon L, McDonald MA, Pollock Bar-Ziv S et al (2013) Chronotropic incompetence, impaired exercise capacity, and inflammation in recipients of continuous-flow left ventricular assist devices. J Heart Lung Transplant 32:930–932
Pruijsten RV, de Jonge N, Kirkels JH, Klöpping C, Doevendans PAFM, Oosterom A, Kemperman H, Lahpor JR (2008) Left ventricular assist device: a functional comparison with heart transplantation. Neth Heart J 16:41–46
Jaski BE, Lingle RJ, Kim J, Branch KR, Goldsmith R, Johnson MR, Lahpor JR, Icenogle TB, Piña I, Adamson R, Favrot LK, Dembitsky WP (1999) Comparison of functional capacity in patients with end-stage heart failure following implantation of a left ventricular assist device versus heart transplantation: results of the experience with left ventricular assist device with exercise trial. J Heart Lung Transplant 18:1031–1040
Gullestad L, Myers J, Edvardsen T, Kjekshus J, Geiran O, Simonsen S (2004) Predictors of exercise capacity and the impact of angiographic coronary artery disease in heart transplant recipients. Am Heart J 147:49–54
Belardinelli R, Georgiou D, Cianci G, Purcaro A (1999) Randomized, controlled trial of long-term moderate exercise training in chronic heart failure: effects on functional capacity, quality of life, and clinical outcome. Circulation 99:1173–1182
Feldman D, Pamboukian SV, Teuteberg JJ, Birks E, Lietz K, Moore SA, Morgan JA, Arabia F, Bauman ME, Buchholz HW, Deng M, Dickstein ML, el-Banayosy A, Elliot T, Goldstein DJ, Grady KL, Jones K, Hryniewicz K, John R, Kaan A, Kusne S, Loebe M, Massicotte MP, Moazami N, Mohacsi P, Mooney M, Nelson T, Pagani F, Perry W, Potapov EV, Eduardo Rame J, Russell SD, Sorensen EN, Sun B, Strueber M, Mangi AA, Petty MG, Rogers J, International Society for Heart and Lung Transplantation (2013) The 2013 International Society for Heart and Lung Transplantation guidelines for mechanical circulatory support: executive summary. J Heart Lung Transplant 32:157–187
Bristow MR, Hershberger RE, Port JD, Gilbert EM, Sandoval A, Rasmussen R, Cates AE, Feldman AM (1990) Beta-adrenergic pathways in nonfailing and failing human ventricular myocardium. Circulation 82:I12–I25
Alsara O, Perez-Terzic C, Squires RW, Dandamudi S, Miranda WR, Park SJ, Thomas RJ (2014) Is exercise training safe and beneficial in patients receiving left ventricular assist device therapy? J Cardiopulm Rehabil Prev 34:233–240
Jung MH, Gustafsson F (2015) Exercise in heart failure patients supported with a left ventricular assist device. J Heart Lung Transplant 34:489–496
Toufik MH, Alok S, Muhammad A, et al. (2016) Effect of cardiac rehabilitation on functional capacity in left ventricular assist device patients: a systematic review and meta-analysis. American Association of Cardiovascular and Pulmonary Rehabilitation 31st Annual Meeting Scientific Abstracts 295–6
Ganga HV, Leung A, Jantz J, Choudhary G, Stabile L, Levine DJ, Sharma SC, Wu WC (2017) Supervised exercise training versus usual care in ambulatory patients with left ventricular assist devices: a systematic review. PLoS One 12:e0174323
Higgins J, Green S, Becker L, et al. (2011) Overviews of reviews. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. http://handbook.cochrane.org/chapter_22/22_overviews_of_reviews.htm (accessed 27 Feb 2015)
Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52:377–384
Adamopoulos S, Gouziouta A, Mantzouratou P, Laoutaris ID, Dritsas A, Cokkinos DV, Mourouzis I, Sfyrakis P, Iervasi G, Pantos C (2013) Thyroid hormone signalling is altered in response to physical training in patients with end-stage heart failure and mechanical assist devices: potential physiological consequences? Interact Cardiovasc Thorac Surg 17:664–668
Compostella L, Russo N, Setzu T, Compostella C, Bellotto F (2014) Exercise performance of chronic heart failure patients in the early period of support by an axial-flow left ventricular assist device as destination therapy. Artif Organs 38:366–373
de Jonge N, Kirkels H, Lahpor JR, Klöpping C, Hulzebos EJ, Brutel de la Rivière A, Robles de Medina EO (2001) Exercise performance in patients with end-stage heart failure after implantation of a left ventricular assist device and after heart transplantation: an outlook for permanent assisting? J Am Coll Cardiol 37:1794–1799
Hayes K, Leet AS, Bradley SJ, Holland AE (2012) Effects of exercise training on exercise capacity and quality of life in patients with a left ventricular assist device: a preliminary randomized controlled trial. J Heart Lung Transplant 31:729–734
Karapolat H, Engin C, Eroglu M, Yagdi T, Zoghi M, Nalbantgil S, Durmaz B, Kirazlı Y, Özbaran M (2013) Efficacy of the cardiac rehabilitation program in patients with end-stage heart failure, heart transplant patients, and left ventricular assist device recipients. Transplant Proc 45:3381–3385
Kerrigan DJ, Williams CT, Ehrman JK, Saval MA, Bronsteen K, Schairer JR, Swaffer M, Brawner CA, Lanfear DE, Selektor Y, Velez M, Tita C, Keteyian SJ (2014) Cardiac rehabilitation improves functional capacity and patient-reported health status in patients with continuous-flow left ventricular assist devices: the rehab-VAD randomized controlled trial. JACC Heart failure 2:653–659
Kohli HS, Canada J, Arena R, Tang DG, Peberdy MA, Harton S, Flattery M, Doolin K, Katlaps GJ, Hess ML, Kasirajan V, Shah KB (2011) Exercise blood pressure response during assisted circulatory support: comparison of the total artificial [corrected] heart with a left ventricular assist device during rehabilitation. J Heart Lung Transplant 30:1207–1213
Kormos RL, Murali S, Dew MA, Armitage JM, Hardesty RL, Borovetz HS, Griffith BP (1994) Chronic mechanical circulatory support: rehabilitation, low morbidity, and superior survival. Ann Thorac Surg 57:51–57 discussion 7-8
Kugler C, Malehsa D, Schrader E, Tegtbur U, Guetzlaff E, Haverich A, Strueber M (2012) A multi-modal intervention in management of left ventricular assist device outpatients: dietary counselling, controlled exercise and psychosocial support. Eur J Cardiothorac Surg 42:1026–1032
Laoutaris ID, Dritsas A, Adamopoulos S, Manginas A, Gouziouta A, Kallistratos MS, Koulopoulou M, Voudris V, Cokkinos DV, Sfirakis P (2011) Benefits of physical training on exercise capacity, inspiratory muscle function, and quality of life in patients with ventricular assist devices long-term postimplantation. Eur J Cardiovasc Prev Rehabil 18:33–40
Marko C, Danzinger G, Kaferback M et al (2015) Safety and efficacy of cardiac rehabilitation for patients with continuous flow left ventricular assist devices. Eur J Prev Cardiol 22:1378–1384
Morrone TM, Buck LA, Catanese KA, Goldsmith RL, Cahalin LP, Oz MC, Levin HR (1996) Early progressive mobilization of patients with left ventricular assist devices is safe and optimizes recovery before heart transplantation. J Heart Lung Transplant 15:423–429
Nakatani T, Sasako Y, Kobayashi J, Komamura K, Kosakai Y, Nakano K, Yamamoto F, Kumon K, Miyatake K, Kitamura S, Takano H (1998) Recovery of cardiac function by long-term left ventricular support in patients with end-stage cardiomyopathy. ASAIO J 44:M516–M520
Sapirstein JS, Pae WE Jr, Aufiero TX, Boehmer JP, Pierce WS (1995) Long-term left ventricular assist device use before transplantation. ASAIO J 41:M530–M534
Wieselthaler GM, Schima H, Dworschak M, Quittan M, Nuhr M, Czerny M, Seebacher G, Huber L, Grimm M, Wolner E (2001) First experiences with outpatient care of patients with implanted axial flow pumps. Artif Organs 25:331–335
Wieselthaler GM, Schima H, Lassnigg AM, Dworschak M, Pacher R, Grimm M, Wolner E (2001) Lessons learned from the first clinical implants of the DeBakey ventricular assist device axial pump: a single center report. Ann Thorac Surg 71:S139–S143 discussion S44-6
Failde I, Ramos I (2000) Validity and reliability of the SF-36 health survey questionnaire in patients with coronary artery disease. J Clin Epidemiol 53:359–365
Bergner M, Bobbitt RA, Carter WB, Gilson BS (1981) The sickness impact profile: development and final revision of a health status measure. Med Care 19:787–805
Green CP, Porter CB, Bresnahan DR, Spertus JA (2000) Development and evaluation of the Kansas City cardiomyopathy questionnaire: a new health status measure for heart failure. J Am Coll Cardiol 35:1245–1255
Rector TS, Cohn JN (1992) Assessment of patient outcome with the Minnesota living with heart failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan multicenter research group. Am Heart J 124:1017–1025
Gitt AK, Wasserman K, Kilkowski C, Kleemann T, Kilkowski A, Bangert M, Schneider S, Schwarz A, Senges J (2002) Exercise anaerobic threshold and ventilatory efficiency identify heart failure patients for high risk of early death. Circulation 106:3079–3084
Cohn JN, Johnson GR, Shabetai R, Loeb H, Tristani F, Rector T, Smith R, Fletcher R (1993) Ejection fraction, peak exercise oxygen consumption, cardiothoracic ratio, ventricular arrhythmias, and plasma norepinephrine as determinants of prognosis in heart failure. The V-HeFT VA cooperative studies group. Circulation 87:VI5–V16
Corra U, Mezzani A, Bosimini E et al (2004) Cardiopulmonary exercise testing and prognosis in chronic heart failure: a prognosticating algorithm for the individual patient. Chest 126:942–950
Lund LH, Aaronson KD, Mancini DM (2005) Validation of peak exercise oxygen consumption and the heart failure survival score for serial risk stratification in advanced heart failure. Am J Cardiol 95:734–741
Piepoli MF, Corra U, Adamopoulos S et al (2014) Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: a policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur J Prev Cardiol 21:664–681
Corra U, Pistono M, Mezzani A et al (2011) Cardiovascular prevention and rehabilitation for patients with ventricular assist device from exercise therapy to long-term therapy. Part I: exercise therapy. Monaldi Arch Chest Dis = Archivio Monaldi per le malattie del torace 76:27–32
Haufe S, Bara C, Eigendorf J, et al. (2017) Physical activity guided by pulse pressure in patients with continuous flow left ventricular assist devices: a pilot study. Circulation 135:1567–1569
Fresiello L, Buys R, Timmermans P, Vandersmissen K, Jacobs S, Droogne W, Ferrari G, Rega F, Meyns B (2016) Exercise capacity in ventricular assist device patients: clinical relevance of pump speed and power. Eur J Cardiothorac Surg 50:752–757
Hayward CS, Fresiello L, Meyns B (2016) Exercise physiology in chronic mechanical circulatory support patients: vascular function and beyond. Curr Opin Cardiol 31:292–298
Acknowledgements
We wish to thank Dr. Dennis J. Kerrigan and Dr. Kate Hayes who kindly provided additional data for the meta-analysis. We also gratefully acknowledge Dr. Susan Marzolini for advice on analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Vivek Rao is a consultant to CorMatrix, and Heart-Ware. The other authors have no conflicts of interest to disclose.
Additional information
What is already known about this subject?
Ventricular assist device (VAD) recipients have persistently reduced functional capacity and hence low quality of life. Early data suggest that exercise rehabilitation may improve both functional capacity and quality of life.
What does this study add?
Through meta-analysis, exercise rehabilitation was shown to result in significantly improved functional capacity (peak VO2 and 6-min walk test distance) when compared to usual care. Benefits were also observed in quality of life and chronotropic responses, but not exercise physiology parameters.
How might this impact on clinical practice?
These results provide support for clinical practice recommendations that VAD recipients receive exercise training. Cardiac rehabilitation societies should develop education programs for professionals to increase capacity to treat this population.
Rights and permissions
About this article
Cite this article
Grosman-Rimon, L., Lalonde, S.D., Sieh, N. et al. Exercise rehabilitation in ventricular assist device recipients: a meta-analysis of effects on physiological and clinical outcomes. Heart Fail Rev 24, 55–67 (2019). https://doi.org/10.1007/s10741-018-9695-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-018-9695-y