Abstract
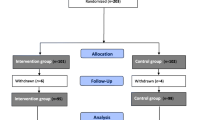
Brief, cost-effective interventions to promote diabetes self-management are needed. This study evaluated the effects of a brief, regular, proactive, telephone “coaching” intervention delivered by paraprofessionals on diabetes adherence, glycemic control, diabetes-related medical symptoms, and depressive symptoms. Therapeutic mechanisms underlying the intervention’s effect on the primary outcomes were also examined. Adults diagnosed with type 2 diabetes (N = 62) were randomly assigned to receive the “coaching” intervention and treatment as usual, or only treatment as usual. The intervention increased frequency of exercise and feet inspection, improved diet, reduced diabetes medical symptoms, and lowered depressive symptoms. Self-efficacy, reinforcement, and awareness of self-care goals mediated the treatment effect on depression, exercise, and feet inspection, respectively. A brief telephone intervention delivered by paraprofessionals had positive effects on type 2 diabetes patients.

Similar content being viewed by others
Notes
The lipid requirements for the present study represent relatively low thresholds. For example, approximately half of all adults have cholesterol levels above 200.
The number of participants completing the social support (n = 31) and reinforcement received (n = 28) was lower than the study N because initial versions of these measures did not adequately direct participants to reflect on support and reinforcement received from their healthcare team. Only responses to the corrected versions were included in analyses of these variables.
References
Anderson, R. J., Freedland, K. E., Clouse, R. E., & Lustman, P. J. (2001). The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care, 24, 1069–1078. doi:10.2337/diacare.24.6.1069.
Apelqvist, J., & Larsson, J. (2000). What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes/Metabolism Research and Reviews, 16(Suppl. 1), S75–S83. doi10.1002/1520-7560(200009/10)16:1+<::AID-DMRR139>3.0.CO;2-8.
Bandura, A. (1998). Health promotion from the perspective of social-cognitive theory. Psychology & Health, 13, 623–649. doi:10.1080/08870449808407422.
Bandura, A., Pastorelli, C., Barbaranelli, C., & Caprara, G. V. (1999). Self-efficacy pathways to childhood depression. Journal of Personality and Social Psychology, 76, 258–269. doi:10.1037/0022-3514.76.2.258.
Brown, S. A. (1990). Studies of educational interventions and outcomes in diabetic adults: A meta-analysis revisited. Patient Education & Counseling, 16(3), 189–215.
Brown, D. W., Balluz, L. S., Giles, W. H., Beckles, G. L., Moriarty, D. G., Ford, E. S., et al. (2004). Diabetes mellitus and health-related quality of life among older adults: Findings from the behavioral risk factor surveillance system (BRFSS). Diabetes Research and Clinical Practice, 65, 105–115. doi:10.1016/j.diabres.2003.11.014.
Carver, C. S., & Scheier, M. F. (1999). Control theory: A useful conceptual framework for personality-social, clinical, and health psychology. In R. F. Baumeister, et al. (Eds.), The self in social psychology (pp. 299–316). Philadelphia: Psychology Press/Taylor & Francis.
Christensen, A., & Jacobson, N. S. (1994). Who (or what) can do psychotherapy: The status and challenge of nonprofessional therapies. Psychological Science, 5, 8–14. doi:10.1111/j.1467-9280.1994.tb00606.x.
Ciechanowski, P. S., Katon, W. J., & Russo, J. E. (2000). Depression and diabetes: Impact of depressive symptoms on adherence, function, and costs. Archives of Internal Medicine, 160, 3278–3283. doi:10.1001/archinte.160.21.3278.
Cowie, C. C., Rust, K. F., Byrd-Holt, D. D., Eberhardt, M. S., Flegal, K. M., Engelgau, M. M., et al. (2006). Prevalence of diabetes and impaired fasting glucose in adults in the US population: National Health and Nutrition Examination Survey 1999–2002. Diabetes Care, 29, 1263–1268. doi:10.2337/dc06-0062.
de Groot, M., Anderson, R., Freedland, K. E., Clouse, R. E., & Lustman, P. J. (2001). Association of depression and diabetes complications: A meta-analysis. Psychosomatic Medicine, 63, 619–630.
DiMatteo, M. (2004). Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care, 42(3), 200–209. doi:10.1097/01.mlr.0000114908.90348.f9.
Eakin, E. G., Lawler, S. P., Vandelanotte, C., & Owen, N. (2007). Telephone interventions for physical activity and dietary behavior change: A systematic review. American Journal of Preventive Medicine, 32, 419–434. doi:10.1016/j.amepre.2007.01.004.
Eddy, D. M., Schlessinger, L., & Kahn, R. (2005). Clinical outcomes and cost-effectiveness of strategies for managing people at high risk for diabetes. Annals of Internal Medicine, 143(4), 251–264.
Egede, L. E., Nietert, P. J., & Zheng, D. (2005). Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care, 28, 1339–1345. doi:10.2337/diacare.28.6.1339.
Engum, A., Mykletun, A., Midthjell, K., Holen, A., & Dahl, A. A. (2005). Depression and diabetes: A large population-based study of sociodemographic, lifestyle, and clinical factors associated with depression in type 1 and type 2 diabetes. Diabetes Care, 28, 1904–1909. doi:10.2337/diacare.28.8.1904.
Fertig, B. J., Simmons, D. A., & Martin, D. B. (1995). Therapy for diabetes. In National Diabetes Data Group (Ed.), Diabetes in America (2nd ed.). Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
Fisher, E., Arfken, C., Heins, J., Houston, C., Jeffe, D., & Sykes, R. (1997). Acceptance of diabetes regimens in adults. In Handbook of health behavior research II: Provider determinants (pp. 189–212). New York: Plenum Press.
Fitzgerald, J. T., Funnell, M. M., Hess, G. E., Barr, P. A., Anderson, R. M., Hiss, R. G., et al. (1998). The reliability and validity of a brief diabetes knowledge test. Diabetes Care, 21(5), 706–710. doi:10.2337/diacare.21.5.706.
Foreyt, J. P., & Poston, W. S. C., I. I. (1999). The challenge of diet, exercise and lifestyle modification in the management of the obese diabetic patient. International Journal of Obesity and Related Metabolic Disorders, 23, S5–S11. doi:10.1038/sj.ijo.0800955.
Friedman, A., Wells, K., Steiner, P., Malone, J., Morrison, A., & Sacco, W. P. (2003). Can a paraprofessional telephone coaching intervention improve exercise and foot care adherence in type 2 diabetes patients? Annals of Behavioral Medicine, 25, S 28.
Gallant, M. P. (2003). The influence of social support on chronic illness self-management: A review and directions for research. Health Education & Behavior, 30, 170–195. doi:10.1177/1090198102251030.
Gilmer, T. P., O’Connor, P. J., Rush, W. A., Lauren Crain, A., Whitebird, R. R., Hanson, A. M., et al. (2005). Predictors of health care costs in adults with diabetes. Diabetes Care, 28, 59–64. doi:10.2337/diacare.28.1.59.
Glasgow, R. E., & Eakin, E. G. (1998). Issues in diabetes self-management. In S. A. Shumaker, E. B. Schron, et al. (Eds.), The handbook of health behavior change (2nd ed., pp. 435–461). New York: Springer Publishing Co.
Glasgow, R. E., Marrero, D., Fisher, E. B., Johnson, S. B., Anderson, B. J., Rubin, R. R., et al. (1999). Behavioral science in diabetes. Diabetes Care, 22, 832–843. doi:10.2337/diacare.22.5.832.
Gollwitzer, P. M. (1999). Implementation intentions: Strong effects of simple plans. The American Psychologist, 54, 493–503. doi:10.1037/0003-066X.54.7.493.
Grootenhuis, P. A., Snoek, F. J., Heine, R. J., & Bouter, L. M. (1994). Development of a Type 2 diabetes symptom checklist: A measure of symptom severity. Diabetic Medicine, 11, 253–261.
Gucciardi, E., De Melo, M., Offenheim, A., Grace, S., & Stewart, D. (2007). Patient factors associated with attrition from a self-management education programme? Journal of Evaluation in Clinical Practice, 13(6), 913–919.
Hattie, J. A., Sharpley, C. F., & Rogers, H. J. (1984). Comparative effectiveness of professional and paraprofessional helpers. Psychological Bulletin, 95, 534–541. doi:10.1037/0033-2909.95.3.534.
King, A., Friedman, R., Marcus, B., Castro, C., Napolitano, M., Ahn, D., et al. (2007). Ongoing physical activity advice by humans versus computers: The Community Health Advice by Telephone (CHAT) Trial. Health Psychology, 26(6), 718–727. doi:10.1037/0278-6133.26.6.718.
Kirkman, M. S., Weinberger, M., Landsman, P. B., Samsa, G. P., Shortliffe, E. A., Simel, D. L., et al. (1994). A telephone-delivered intervention for patients with NIDDM: Effect on coronary risk factors. Diabetes Care, 17(8), 840–846. doi:10.2337/diacare.17.8.840.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi:10.1046/j.1525-1497.2001.016009606.x.
Landell-Graham, J., Yount, S. E., & Rudnicki, S. R. (2003). Diabetes mellitus. In A. M. Nezu, C. M. Nezu, & P. A. Geller (Eds.), Health psychology. I. B. Weiner (Series Ed.), Handbook of psychology, (Vol. 9). New York: John Wiley & Sons.
Ludman, E. J., Katon, W., Russo, J., Von Korff, M., Simon, G., Ciechanowski, P., et al. (2004). Depression and diabetes symptom burden. General Hospital Psychiatry, 26, 430–436. doi:10.1016/j.genhosppsych.2004.08.010.
MacKinnon, D. P., Lockwood, M., Hoffman, J. M., West, S. G., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104. doi:10.1037/1082-989X.7.1.83.
Mensing, C., et al. (2002). National standards for diabetes self-management education. Diabetes Care, 25S, S140–S147. doi:10.2337/diacare.25.2007.S140.
Norris, S. L., Engelgau, M. M., & Narayan, K. M. (2001). Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care, 24, 561–587. doi:10.2337/diacare.24.3.561.
Ortegon, M. M., Redekop, W. K., & Niessen, L. W. (2004). Cost-effectiveness of prevention and treatment of the diabetic foot: A Markov analysis. Diabetes Care, 27(4), 901–907. doi:10.2337/diacare.27.4.901.
Penninx, B., van Tilburg, T., Boeke, A., Deeg, D., Kriegsman, D., & van Eijk, J. (1998). Effects of social support and personal coping resources on depressive symptoms: Different for various chronic diseases? Health Psychology, 17, 551–558. doi:10.1037/0278-6133.17.6.551.
Piette, J. D., Weinberger, M., McPhee, S. J., Mah, C. A., Kraemer, F. B., & Crapo, L. M. (2000). Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? The American Journal of Medicine, 108(1), 20–27. doi:10.1016/S0002-9343(99)00298-3.
Pinto, B., Friedman, R., Marcus, B., Kelley, H., Tennstedt, S., & Gillman, M. (2002). Effects of a computer-based, telephone-counseling system on physical activity. American Journal of Preventive Medicine, 23(2), 113–120. doi:10.1016/S0749-3797(02)00441-5.
Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in simple and multiple mediator models. Behavior Research Methods, 40, 879–891. doi:10.3758/BRM.40.3.879.
Sacco, W. P., & Beck, A. T. (1995). Cognitive theory and therapy. In E. Edward Beckham & W. R. Leber (Eds.), Handbook of depression: Treatment, assessment and research (2nd ed., pp. 329–351). New York: Guilford Press.
Sacco, W. P., Morrison, A. D., & Malone, J. I. (2004). A brief, regular, proactive telephone coaching intervention for diabetes: Rationale, description, and preliminary results. Journal of Diabetes and Its Complications, 18, 113–118. doi:10.1016/S1056-8727(02)00254-4.
Sacco, W. P., Wells, K. J., Friedman, A., Matthew, R., Perez, S., & Vaughan, C. A. (2007). Adherence, BMI, and depression in adults with type 2 diabetes: The mediational role of diabetes symptoms and self-efficacy. Health Psychology, 26, 693–700.
Sacco, W., Wells, K., Vaughan, C., Friedman, A., Perez, S., & Matthew, R. (2005). Depression in adults with type 2 diabetes: The role of adherence, body mass index, and self-efficacy. Health Psychology, 24(6), 630–634. doi:10.1037/0278-6133.24.6.630.
Sacco, W. P., & Yanover, T. (2006). Diabetes and depression: The role of social support and medical symptoms. Journal of Behavioral Medicine, 29, 523–531. doi:10.1007/s10865-006-9072-5.
Schafer, J. L. (1999). NORM: Multiple imputation of incomplete multivariate data under a normal model, version 2. Software for Windows 95/98/NT, available from http://www.stat.psu.edu/~jls/misoftwa.html.
Sigal, R. J., Kenny, G. P., Wasserman, D. H., Castaneda-Sceppa, C., & White, R. D. (2006). Physical activity/exercise and Type 2 diabetes: A consensus statement from the American Diabetes Association. Diabetes Care, 29, 1433–1438. doi:10.2337/dc06-9910.
Simon, G. E., Katon, W. J., Lin, E. H. B., Rutter, C., Manning, W. G., Von Korff, M., et al. (2007). Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Archives of General Psychiatry, 64, 65–72. doi:10.1001/archpsyc.64.1.65.
Snowling, N. J., & Hopkins, W. G. (2006). Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: A meta-analysis. Diabetes Care, 29(11), 2518–2527. doi:10.2337/dc06-1317.
Sobel, M. E. (1982). Asymptotic intervals for indirect effects in structural equations models. In S. Leinghart (Ed.), Sociological methodology (pp. 290–312). San Francisco: Jossey-Bass.
Spitzer, R. L., Kroenke, K., Williams, J. B., & The Patient Health Questionnaire Primary Care Study Group. (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of the American Medical Association, 282, 1737–1744. doi:10.1001/jama.282.18.1737.
Talbot, R., Nouwen, A., Gingras, J., Gosselin, M., & Audet, J. (1997). The assessment of diabetes-related cognitive and social factors: The multidimensional diabetes questionnaire. Journal of Behavioral Medicine, 20, 291–312. doi:10.1023/A:1025508928696.
Thomas, D. E., Elliott, E. J., & Naughton, G. A. (2006). Exercise for type 2 diabetes mellitus. The Cochrane Database of Systematic Reviews, 3, CD002968.
Toobert, D. J., & Glasgow, R. E. (1994). Assessing diabetes self management: The summary of diabetes self-care activities questionnaire. In C. Bradley (Ed.), Handbook of psychology and diabetes (pp. 351–375). Chur, Switzerland: Harwood Academic.
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23, 943–949. doi:10.2337/diacare.23.7.943.
van Dam, H. A., van der Horst, F. G., Knoops, L., Ryckman, R. M., Crebolder, H. F., & van den Borne, B. H. (2005). Social support in diabetes: A systematic review of controlled intervention studies. Patient Education and Counseling, 59, 1–12. doi:10.1016/j.pec.2004.11.001.
Watkins, K. W., Connell, C. M., Fitzgerald, J. T., Klem, L., Hickey, T., & Ingersoll-Dayton, B. (2000). Effect of adults’ self-regulation of diabetes on quality-of-life outcomes. Diabetes Care, 23(10), 1511–1515. doi:10.2337/diacare.23.10.1511.
Watson, D., & Pennebaker, J. W. (1989). Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychological Bulletin, 96, 234–254.
Weinberger, M., Kirkman, M. S., Samsa, G. P., Shortliffe, E. A., Landsman, P. B., Cowper, P. A., et al. (1995). A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: Impact on glycemic control and health-related quality of life. Journal of General Internal Medicine, 10(2), 59–66. doi:10.1007/BF02600227.
Whitlock, W. L., Brown, A., Moore, K., Pavliscsak, H., Dingbaum, A., Lacefield, D., et al. (2000). Telemedicine improved diabetic management. Military Medicine, 165(8), 579–584.
Acknowledgments
This research was supported, in part, by an Award from the American Heart Association. The authors acknowledge the following individuals who served as coaches for this study: Amanda Magee, Laura Cardona, Rebecca Mathew, Barbara Houser, Kristin Phillips, Patricia Steiner, Claudia Gerard, Ariz Rojas, Antoniette Maldonado, Nicole Bower, and Tenille Valdivia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Preliminary results from this study were previously presented (Friedman et al. 2003).
Rights and permissions
About this article
Cite this article
Sacco, W.P., Malone, J.I., Morrison, A.D. et al. Effect of a brief, regular telephone intervention by paraprofessionals for type 2 diabetes. J Behav Med 32, 349–359 (2009). https://doi.org/10.1007/s10865-009-9209-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-009-9209-4