Abstract
Purpose
To facilitate MRI-guided catheterization procedures, we present an MRI-compatible remote catheter navigation system that allows remote navigation of steerable catheters with 3 degrees of freedom.
Methods
The system consists of a user interface (master), a robot (slave), and an ultrasonic motor control servomechanism. The interventionalist applies conventional motions (axial, radial and plunger manipulations) on an input catheter in the master unit; this user input is measured and used by the servomechanism to control a compact catheter manipulating robot, such that it replicates the interventionalist’s input motion on the patient catheter. The performance of the system was evaluated in terms of MRI compatibility (SNR and artifact), feasibility of remote navigation under real-time MRI guidance, and motion replication accuracy.
Results
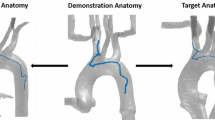
Real-time MRI experiments demonstrated that catheter was successfully navigated remotely to desired target references in all 3 degrees of freedom. The system had an absolute value error of \({<}\)1 mm in axial catheter motion replication over 30 mm of travel and \(3^{\circ } \pm 2^{\circ }\) for radial catheter motion replication over \(180^{\circ }\). The worst case SNR drop was observed to be \({<}\)3 %; the robot did not introduce any artifacts in the MR images.
Conclusion
An MRI-compatible compact remote catheter navigation system has been developed that allows remote navigation of steerable catheters with 3 degrees of freedom. The proposed system allows for safe and accurate remote catheter navigation, within conventional closed-bore scanners, without degrading MR image quality.






Similar content being viewed by others
References
Lickfett L, Mahesh M, Vasamreddy C, Bradley D, Jayam V, Eldadah Z, Dickfeld T, Kearney D, Dalal D, Luderitz B, Berger R, Calkins H (2004) Radiation exposure during catheter ablation of atrial fibrillation. Circulation 110(19):3003–3010. doi:10.1161/01.CIR.0000146952.49223.11
Perisinakis K, Damilakis J, Theocharopoulos N, Manios E, Vardas P, Gourtsoyiannis N (2001) Accurate assessment of patient effective radiation dose and associated detriment risk from radiofrequency catheter ablation procedures. Circulation 104(1):58–62
Pantos I, Patatoukas G, Katritsis DG, Efstathopoulos E (2009) Patient radiation doses in interventional cardiology procedures. Curr Cardiol Rev 5(1):1–11. doi:10.2174/157340309787048059
Klein LW, Miller DL, Balter S, Laskey W, Haines D, Norbash A, Mauro MA, Goldstein JA, Joint Inter-Society Task Force on Occupational Hazards in the Interventional L (2009) Occupational health hazards in the interventional laboratory: time for a safer environment. Catheter Cardiovasc Interv 73(3):432–438. doi:10.1002/ccd.21801
Roguin A, Goldstein J, Bar O (2012) Brain tumours among interventional cardiologists: a cause for alarm? Report of four new cases from two cities and a review of the literature. Eurointervention 7(9):1081–1086
Faddis MN, Blume W, Finney J, Hall A, Rauch J, Sell J, Bae KT, Talcott M, Lindsay B (2002) Novel, magnetically guided catheter for endocardial mapping and radiofrequency catheter ablation. Circulation 106(23):2980–2985
Faddis MN, Chen J, Osborn J, Talcott M, Cain ME, Lindsay BD (2003) Magnetic guidance system for cardiac electrophysiology: a prospective trial of safety and efficacy in humans. J Am Coll Cardiol 42(11):1952–1958
Saliba W, Cummings JE, Oh S, Zhang Y, Mazgalev TN, Schweikert RA, Burkhardt JD, Natale A (2006) Novel robotic catheter remote control system: feasibility and safety of transseptal puncture and endocardial catheter navigation. J Cardiovasc Electrophysiol 17(10):1102–1105. doi:10.1111/j.1540-8167.2006.00556.x
Saliba W, Reddy VY, Wazni O, Cummings JE, Burkhardt JD, Haissaguerre M, Kautzner J, Peichl P, Neuzil P, Schibgilla V, Noelker G, Brachmann J, Di Biase L, Barrett C, Jais P, Natale A (2008) Atrial fibrillation ablation using a robotic catheter remote control system: initial human experience and long-term follow-up results. J Am Coll Cardiol 51(25):2407–2411. doi:10.1016/J.Jacc.2008.03.027
Beyar R, Wenderow T, Lindner D, Kumar G, Shofti R (2005) Concept, design and pre-clinical studies for remote control percutaneous coronary interventions. Eurointervention 1(3):340–345
Khan EM, Frumkin W, Ng GA, Neelagaru S, Abi-Samra FM, Lee J, Giudici M, Gohn D, Winkle RA, Sussman J, Knight BP, Berman A, Calkins H (2013) First experience with a novel robotic remote catheter system: Amigo mapping trial. J Interv Card Electrophysiol 37(2):121–129. doi:10.1007/s10840-013-9791-9
Ullah W, McLean A, Hunter RJ, Baker V, Richmond L, Cantor EJ, Dhinoja MB, Sporton S, Earley MJ, Schilling RJ (2014) Randomized trial comparing robotic to manual ablation for atrial fibrillation. Heart Rhythm 11(11):1862–1869. doi:10.1016/j.hrthm.2014.06.026
Dinov B, Schonbauer R, Wojdyla-Hordynska A, Braunschweig F, Richter S, Altmann D, Sommer P, Gaspar T, Bollmann A, Wetzel U, Rolf S, Piorkowski C, Hindricks G, Arya A (2012) Long-term efficacy of single procedure remote magnetic catheter navigation for ablation of ischemic ventricular tachycardia: a retrospective study. J Cardiovasc Electrophysiol 23(5):499–505. doi:10.1111/j.1540-8167.2011.02243.x
Wijnmaalen AP, van der Geest RJ, van Huls van Taxis CF, Siebelink HM, Kroft LJ, Bax JJ, Reiber JH, Schalij MJ, Zeppenfeld K (2011) Head-to-head comparison of contrast-enhanced magnetic resonance imaging and electroanatomical voltage mapping to assess post-infarct scar characteristics in patients with ventricular tachycardias: real-time image integration and reversed registration. Eur Heart J 32(1):104–114. doi:10.1093/eurheartj/ehq345
Radau PE, Pintilie S, Flor R (2012) VURTIGO: visualization platform for real-time, MRI-Guided cardiac electroanatomic mapping. In: Statistical atlases and computational models of the heart. Imaging and modelling challenges, vol 7085. 1 edn., pp 244–253
Lardo AC, McVeigh ER, Jumrussirikul P, Berger RD, Calkins H, Lima J, Halperin HR (2000) Visualization and temporal/spatial characterization of cardiac radiofrequency ablation lesions using magnetic resonance imaging. Circulation 102(6):698–705
Ranjan R, Kholmovski EG, Blauer J, Vijayakumar S, Volland NA, Salama ME, Parker DL, MacLeod R, Marrouche NF (2012) Identification and acute targeting of gaps in atrial ablation lesion sets using a real-time magnetic resonance imaging system. Circ Arrhythm Electrophysiol 5(6):1130–1135. doi:10.1161/circep.112.973164
Zia MI, Ghugre NR, Connelly KA, Strauss BH, Sparkes JD, Dick AJ, Wright GA (2012) Characterizing myocardial edema and hemorrhage using quantitative T2 and T2* mapping at multiple time intervals post ST-segment elevation myocardial infarction. Circ-Cardiovasc Imaging 5(5):566–572
Bhagirath P, van der Graaf M, Karim R, Rhode K, Piorkowski C, Razavi R, Schwitter J, Gotte M (2015) Interventional cardiac magnetic resonance imaging in electrophysiology: advances toward clinical translation. Circ-Arrhythm Electrophysiol 8(1):203–211. doi:10.1161/CIRCEP.114.002371
Akoum N, Daccarett M, McGann C, Segerson N, Vergara G, Kuppahally S, Badger T, Burgon N, Haslam T, Kholmovski E, Macleod R, Marrouche N (2011) Atrial fibrosis helps select the appropriate patient and strategy in catheter ablation of atrial fibrillation: a DE-MRI guided approach. J Cardiovasc Electrophysiol 22(1):16–22. doi:10.1111/j.1540-8167.2010.01876.x
Arujuna A, Karim R, Caulfield D, Knowles B, Rhode K, Schaeffter T, Kato B, Rinaldi CA, Cooklin M, Razavi R, O’Neill MD, Gill J (2012) Acute pulmonary vein isolation is achieved by a combination of reversible and irreversible atrial injury after catheter ablation evidence from magnetic resonance imaging. Circ-Arrhythm Electrophysiol 5(4):691–700
Harrison JL, Jensen HK, Peel SA, Chiribiri A, Grondal AK, Bloch LO, Pedersen SF, Bentzon JF, Kolbitsch C, Karim R, Williams SE, Linton NW, Rhode KS, Gill J, Cooklin M, Rinaldi CA, Wright M, Kim WY, Schaeffter T, Razavi RS, O’Neill MD (2014) Cardiac magnetic resonance and electroanatomical mapping of acute and chronic atrial ablation injury: a histological validation study. Eur Heart J 35(22):1486–1495
Uecker M, Zhang S, Voit D, Karaus A, Merboldt KD, Frahm J (2010) Real-time MRI at a resolution of 20 ms. NMR Biomed 23(8):986–994
Nayak KS, Cunningham CH, Santos JM, Pauly JM (2004) Real-time cardiac MRI at 3 tesla. Magn Reson Med 51(4):655–660
Ratnayaka K, Faranesh AZ, Guttman MA, Kocaturk O, Saikus CE, Lederman RJ (2008) Interventional cardiovascular magnetic resonance: still tantalizing. J Cardiovasc Magn Reson 10:62. doi:10.1186/1532-429X-10-62
Tavallaei MA, Thakur Y, Haider S, Drangova M (2013) A magnetic-resonance-imaging-compatible remote catheter navigation system. IEEE Trans Bio Eng 60(4):899–905. doi:10.1109/TBME.2012.2229709
Tavallaei MA, Gelman D, Lavdas MK, Skanes AC, Jones DL, Bax JS, Drangova M (2015) Design, development and evaluation of a compact tele-robotic catheter navigation system. IJMRCAS. doi:10.1002/rcs.1711
Thakur Y, Holdsworth DW, Drangova M (2009) Characterization of catheter dynamics during percutaneous transluminal catheter procedures. IEEE Trans Bio Eng 56(8):2140–2143. doi:10.1109/TBME.2008.921148
Anderson KJ, Scott GC, Wright GA (2012) Catheter tracking with phase information in a magnetic resonance scanner. IEEE Trans Med Imaging 31(6):1173–1180. doi:10.1109/TMI.2011.2179944
Yao W, Schaeffter T, Seneviratne L, Althoefer K (2012) Developing a magnetic resonance-compatible catheter for cardiac catheterization. J Med Devices 6(4). doi:10.1115/1.4007281
Losey AD, Lillaney P, Martin AJ, Halbach VV, Cooke DL, Dowd CF, Higashida RT, Saloner DA, Wilson MW, Saeed M, Hetts SW (2014) Safety of retained microcatheters: an evaluation of radiofrequency heating in endovascular microcatheters with nitinol, tungsten, and polyetheretherketone braiding at 1.5 T and 3 T. J Neurointerventional Surg 6(4):314–319. doi:10.1136/neurintsurg-2013-010746
Tavallaei MA, Drangova M (2015) Patent application: ultrasonic motor control system and method, 24 Sept 2015
Tavallaei MA, Atashzar SF, Drangova M (2015) Robust motion control of ultrasonic motors under temperature disturbance. IEEE Trans Ind Elect. doi:10.1109/TIE.2015.2499723
NEMA (2008) Determination of signal-to-noise ratio (SNR) in diagnostic magnetic resonance imaging, vol MS 1. National Electrical Manufacturers Association
ASTM (2006) F2119-07. Standard test method for evaluation of MR image artifacts from passive implants. ASTM International, West Conshohocken, PA, USA
Tavallaei MA, Johnson P, Liu J, Drangova M (2015) Design and evaluation of an MRI-compatible linear motion stage. Med Phys. doi:10.1118/1.4937780
Hilbert S, Sommer P, Gutberlet M, Gaspar T, Foldyna B, Piorkowski C, Weiss S, Lloyd T, Schnackenburg B, Krueger S, Fleiter C, Paetsch I, Jahnke C, Hindricks G, Grothoff M (2015) Real-time magnetic resonance-guided ablation of typical right atrial flutter using a combination of active catheter tracking and passive catheter visualization in man: initial results from a consecutive patient series. Europace. doi:10.1093/europace/euv249
Vergara GR, Vijayakumar S, Kholmovski EG, Blauer JJE, Guttman MA, Gloschat C, Payne G, Vij K, Akoum NW, Daccarett M, McGann CJ, MacLeod RS, Marrouche NF (2011) Real-time magnetic resonance imaging-guided radiofrequency atrial ablation and visualization of lesion formation at 3 Tesla. Heart Rhythm 8(2):295–303
Grothoff M, Piorkowski C, Eitel C, Gaspar T, Lehmkuhl L, Lucke C, Hoffmann J, Hildebrand L, Wedan S, Lloyd T, Sunnarborg D, Schnackenburg B, Hindricks G, Sommer P, Gutberlet M (2014) MR imaging-guided electrophysiological ablation studies in humans with passive catheter tracking: initial results. Radiology 271(3):695–702. doi:10.1148/radiol.13122671
Campbell-Washburn AE, Rogers T, Xue H, Hansen MS, Lederman RJ, Faranesh AZ (2014) Dual echo positive contrast bSSFP for real-time visualization of passive devices during magnetic resonance guided cardiovascular catheterization. J Cardiovasc Mag Res 16:88. doi:10.1186/s12968-014-0088-7
Acknowledgments
Funding for this work was provided by the Canadian Institutes of Health Research and the Ontario Research Fund. The authors thank Ayda Bashiri and Hristo N. Nikolov for help in the MRI evaluation experiments and Dr. Kevan Anderson for his constructive instructions on catheter modification and development. M.T. and D.G. acknowledge the support of the NSERC Collaborative Research and Training Experience (CREATE) Program in Computer-Assisted Medical Interventions (CAMI) at the University of Western Ontario. M.D. is a Career Investigator of the Heart and Stroke Foundation of Ontario.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (mp4 8892 KB)
Rights and permissions
About this article
Cite this article
Tavallaei, M.A., Lavdas, M.K., Gelman, D. et al. Magnetic resonance imaging compatible remote catheter navigation system with 3 degrees of freedom. Int J CARS 11, 1537–1545 (2016). https://doi.org/10.1007/s11548-015-1337-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-015-1337-4