Abstract
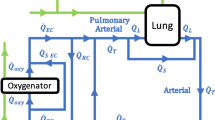
Acute respiratory distress syndrome (ARDS) is a pulmonary edemic condition which reduces respiratory exchange in 150,000 people per year in the United States. The currently available therapies of mechanical ventilation and extracorporeal membrane oxygenation are associated with high mortality rates, so intravenous oxygenation represents an attractive, alternative support modality. We are developing an intravenous membrane oxygenator (IMO) device intended to provide 50% of basal oxygen and carbon dioxide exchange requirements for ARDS patients. A unique aspect of the IMO is its use of an integral balloon to provide active mixing. This paper describes a mathematical model which was developed to quantify and optimize the gas exchange performance of the IMO. The model focuses on balloon activated mixing, uses a lumped compartment approach, and approximates the blood-side mass transfer coefficients with cross-flow correlations. IMO gas exchange was simulated in water and blood, for a variety of device geometries and balloon pulsation rates. The modeling predicts the following: (1) gas exchange efficiency is reduced by a buildup of oxygen in the fluid near the fibers; (2) the IMO gas exchange rate in blood is normally about twice that in water under comparable conditions; (3) a balloon diameter of about 1.5 cm leads to optimal gas exchange performance; and (4) in vivo positioning can affect gas exchange rates. The numerically predicted gas transfer rates correlate closely with those experimentally measured in vitro for current IMO prototypes. © 1998 Biomedical Engineering Society.
PAC98: 8710+e, 8790+y, 8265Fr
Similar content being viewed by others
REFERENCES
Ahmed, T., and M. J. Semmens. Use of transverse flow hollow fibers for bubbleless membrane aeration. Water Res.30:440-446, 1996.
Conrad, S. A., et al.Major findings from the clinical trials of the intravascular oxygenator. Artif. Organs18:846-863, 1994.
Fazzalari, F. L., R. H. Bartlett, M. R. Bonnell, and J. P. Montoya. An intrapleural lung prosthesis: Rationale, design, and testing. Artif. Organs18:801-805, 1994.
4 Federspiel, W. J., T., Hewitt, M. S. Hout, F. R. Walters, L. W. Lund, P. I. Sawzik, G. Reeder, H. S. Borovetz, and B. G. Hattler. Recent progress in engineering the Pittsburgh intravenous membrane oxygenator. ASAIO J.42:M435-M442, 1996.
Fujii, Y., and S. Kigoshi. Characterization of hollow fiber membranes. J. Chem. En. J.27:321-328, 1994.
Gattinoni, L., A. Pesenti, and G. P. Rossi. Treatment of acute respiratory failure with low-frequency positive-pressure ventilation and extracorporeal removal of CO2. Lancet2:292- 294, 1980.
Ichiba, S., and R. H. Bartlett. Current status of extracorporeal membrane oxygenation for severe respiratory failure. Artif. Organs20:120-123, 1996.
Incropera, F. P., and D. P. DeWitt. Introduction to Heat Transfer. New York: Wiley, 1990.
Lund, L. W. Evaluation of flow visualization methods as a design tool for artificial lung development. Carnegie Mellon University, Masters thesis, 1992.
Macha, M., W. J., Federspiel, L. W. Lund, P. J. Sawzik, P. Litwak, F. P. Walters, G. D. Reeder, H. S. Borovetz, and B. G. Hattler. Acute in vivostudies of the Pittsburgh intravenous membrane oxygenator. ASAIO J.42:M609-M615, 1996.
Makarewicz, A. J. Static and dynamic artificial lungs. Ph.D. thesis, Northwestern University, 1994.
Mockros, L. F., and R. Leonard. Compact cross-flow tubular oxygenators. Trans. Am. Soc. Artif. Intern. Organs31:628- 632, 1985.
Mortensen, J. D. Intravascular oxygenator: A new alternative method for augmenting blood gas transfer in patients with acute respiratory failure. Artif. Organs16:75-82, 1992.
Niranjan, S. C., J. W. Clark, K. Y. San, J. B. Zwischenberger, and A. Bidani. Analysis of factors affecting gas exchange in intravascular blood gas exchanger. J. Appl. Physiol.77:1716-1730, 1994.
Pesenti, A., L. Gattinoni, T. Kobolow, and G. Damia. Extracorporeal circulation in adult respiratory failure. ASAIO Trans.34:43-47, 1988.
Snider, M. T., D. B. Campbell, W. A. Kofke, K. M. High, G. B. Russell, M. F. Keamy, and D. R. Williams. Venovenous perfusion of adult and children with severe acute respiratory distress syndrome. ASAIO Trans.34:1014-1020, 1988.
Vaslef, S. N., K. E. Cook, R. J. Leonard, L. F. Mockros, and R. W. Anderson. Design and evaluation of a new, low pressure loss, implantable artificial lung. ASAIO J.40:M522- M526, 1994.
Vaslef, S. N., R. W. Anderson, and R. J. Leonard. Use of a mathematical model to predict oxygen transfer rates in hollow fiber membrane oxygenators. ASAIO J.40:990-996, 1994.
Weinberger, S. E. Principles of Pulmonary Medicine. Philadelphia: Saunders, 1992.
Wickramasinghe, S. R., M. J. Semmens, and E. L. Cussler. Mass transfer in various hollow fiber geometries. J. Membr. Sci.69:235-250, 1992.
Yang, M. C., and E. L. Cussler. Designing hollow fiber contactors. AIChE. J.32:1910-1916 1986.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hewitt, T.J., Hattler, B.G. & Federspiel, W.J. A Mathematical Model of Gas Exchange in an Intravenous Membrane Oxygenator. Annals of Biomedical Engineering 26, 166–178 (1998). https://doi.org/10.1114/1.53
Issue Date:
DOI: https://doi.org/10.1114/1.53