Summary
Abstract|
Echinocandins are a new class of antifungal agents with a novel mechanism of action (interference with fungal cell wall synthesis). Caspofungin (Cancidas®, Caspofungin MSD®) is the first echinocandin to be approved and is administered intravenously.
Caspofungin 50 mg/day had similar efficacy to intravenous fluconazole 200 mg/day and was at least as effective as intravenous amphotericin B 0.5 mg/kg/day in patients with oesophageal candidiasis in two randomised, double-blind studies. A favourable combined clinical and endoscopic response occurred in 81% of caspofungin recipients versus 85% of fluconazole recipients and in 74% of caspofungin recipients versus 63% of amphotericin B recipients. A favourable combined response rate of ≈90% and ≈60% occurred in the stratum of patients with oesophageal candidiasis who received caspofungin or amphotericin B in a third randomised, double-blind study.
Caspofungin (70mg loading dose followed by 50 mg/day) had similar efficacy to intravenous amphotericin B (0.7–1.0 mg/kg/day in patients with neutropenia and 0.6–0.7 mg/kg/day in patients without neutropenia) in patients with invasive candidiasis in a double-blind, randomised trial. A favourable overall response occurred in 73.4% of caspofungin recipients and in 61.7% of amphotericin B recipients.
In a noncomparative study, salvage therapy with caspofungin (70mg loading dose followed by 50 mg/day) was effective in patients with invasive aspergillosis who were refractory to or did not tolerate standard antifungal therapy. A favourable response (complete plus partial response) occurred in 37 of 83 patients (45%).
Caspofungin was generally well tolerated in clinical trials; it had similar tolerability to intravenous fluconazole and was better tolerated than intravenous amphotericin B. Significantly fewer caspofungin than amphotericin B recipients reported chills, fever, nausea or infusion-related adverse events.
In conclusion, caspofungin is a valuable new antifungal agent with a novel mechanism of action. In comparative trials, caspofungin had similar efficacy to fluconazole and was at least as effective as amphotericin B in oesophageal candidiasis and had similar efficacy to amphotericin B in invasive candidiasis. In addition, caspofungin had similar tolerability to fluconazole and was better tolerated than amphotericin B in these indications. Caspofungin was also effective in patients with invasive aspergillosis who were refractory to or intolerant of standard antifungal agents. Thus, caspofungin provides an alternative to triazoles or amphotericin B in oesophageal candidiasis and an alternative to amphotericin B in invasive candidiasis, as well as being an effective salvage therapy in invasive aspergillosis.
Pharmacodynamic Properties
Caspofungin inhibits the synthesis of β-(1,3)-D-glucan, an essential component of the cell wall of many fungi. Thus, by inhibiting β-(1,3)-D-glucan synthase, caspofungin interferes with fungal cell wall synthesis.
Caspofungin has fungicidal activity against Candida spp. in vitro. In one study, caspofungin demonstrated fungicidal activity against Candida albicans and C. tropicalis within 6–8 hours at concentrations that were 0.5–2 times the minimum inhibitory concentration (MIC); another study revealed that the activity of caspofungin was concentration dependent. Numerous studies demonstrated that caspofungin had in vitro activity against clinically significant Candida spp. (e.g. C. albicans, C. krusei, C. tropicalis, C. pseudotropicalis, C. glabrata, C. parapsilosis, C. lusitaniae, C. guilliermondii and C. dubliniensis), including both azole-sensitive and -resistant Candida spp. and amphotericin B-resistant Candida spp. Caspofungin was active against azole-resistant Candida spp. such as C. glabrata and C. krusei, but was less active against C. parapsilosis and C. guilliermondii. For various Candida spp. isolated from patients with invasive candidiasis, the caspofungin MIC ranged from 0.125 to >8 μg/mL. Caspofungin reduced the fungal tissue burden and prolonged survival in animal models of disseminated candidiasis (including immunocompetent and immunocompromised mice and rabbits).
Caspofungin showed in vitro activity against various Aspergillus spp., including Aspergillus flavus, A. fumigatus, A. niger and A. terreus. For Aspergillus isolates obtained from patients involved in clinical trials, 24-hour MIC values at which 80% growth inhibition occurred were <1 μg/mL for all isolates. Staining studies suggest that caspofungin causes lysis of actively growing A. fumigatus cells at the hyphal tips and branch points, although subapical cells with mature cell walls were less susceptible to lysis. Intraperitoneal caspofungin prolonged survival in immunocompromised mice and guinea pigs with disseminated aspergillosis. Results concerning the effect of caspofungin on residual fungal burden were mixed. Administering caspofungin to neutropenic rabbits for the prevention or treatment of pulmonary aspergillosis prolonged survival and reduced A. fumigatus-mediated pulmonary injury. However, the residual fungal burden in the lungs did not change and galactomannan antigenaemia increased.
The results of both in vitro and animal studies suggest potential benefits from combining caspofungin with amphotericin B or azoles in both candidiasis and aspergillosis.
Pharmacokinetic Properties
Unless stated otherwise, pharmacokinetic studies were conducted in healthy volunteers. Administration of single doses of caspofungin 5–100mg resulted in dose-proportional increases in the area under the plasma concentration-time curve from time zero to infinity (AUC0-∞) and in the plasma concentration 1 hour (C1h) and 24 hours (C24h; trough concentration) post-dose. Repeat administration of caspofungin suggested modest pharmacokinetic nonlinearity. Moderate accumulation of caspofungin occurred with repeat administration. Steady state was reached at about week 3. Administration of caspofungin 50 mg/day resulted in C24h values of <1 μg/mL on day 1 and >1 μg/mL (proposed target concentration in invasive infections; derived from in vitro susceptibility testing of Candida spp.) on day 14. Administration of a 70mg loading dose of caspofungin followed by 50 mg/day resulted in a C24h value of >1 μg/mL on both days 1 and 14. Caspofungin plasma concentrations decline in a polyphasic manner. It has a short α-phase of 1–2 hours (volume of distribution of 9.7L) and a β-phase half-life (t1/2) of ≈9–11 hours. The clearance of caspofungin from plasma is primarily influenced by distribution.
Caspofungin is slowly metabolised by hydrolysis and N-acetylation; the drug also undergoes spontaneous chemical degradation. Plasma clearance was 9.85–12.43 mL/min and renal clearance was very slow (0.16 mL/min). Twenty-seven days after administration of a single dose of radiolabelled caspofungin, 41% of the dose had been excreted in the urine and 35% had been excreted in the faeces. Approximately 2% of the dose was recovered in the urine as unchanged drug. The γ-phase t1/2 was 40–50 hours.
The AUC0-∞ of caspofungin was increased by ≈76% in patients with moderate hepatic impairment (Child-Pugh score 7–9) compared with healthy controls following administration of a single 70mg dose of the drug. Administration of a 70mg loading dose of caspofungin followed by 35 mg/day to patients with moderate hepatic impairment only increased the AUC24h on day 14 by 7% compared with healthy controls.
At clinically relevant concentrations, caspofungin does not inhibit any enzyme in the cytochrome P450 (CYP) system or induce the metabolism of other drugs via CYP3A4. Caspofungin does not act as a substrate for P-glycoprotein and is a poor substrate for CYP enzymes. Caspofungin pharmacokinetics were altered by the coadministration of cyclosporin or rifampicin (rifampin) [≈35% increase in AUC and 30% reduction in trough concentration, respectively]. Coadministration of caspofungin and efavirenz, nevirapine, phenytoin, dexamethasone or carbamazepine (inducers of drug clearance) may result in clinically significant reductions in caspofungin concentrations. The whole blood AUC12h of tacrolimus was reduced by ≈20% with concomitant administration of caspofungin, although caspofungin pharmacokinetics were not altered by tacrolimus.
Clinical Efficacy
Studies have evaluated the efficacy of caspofungin in oesophageal candidiasis, invasive candidiasis and invasive aspergillosis. Study drugs in these trials were administered intravenously.
In two randomised, double-blind studies, caspofungin 50 mg/day had similar efficacy to fluconazole 200 mg/day and was at least as effective as amphotericin B 0.5 mg/kg/day in patients with oesophageal candidiasis. A favourable combined clinical and endoscopic response occurred in 81% of caspofungin recipients and 85% of fluconazole recipients 5–7 days after the end of treatment; caspofungin was shown to be noninferior to fluconazole. Four weeks after stopping treatment, the relapse rate was 28% in caspofungin recipients and 17% in fluconazole recipients. In the other study, a favourable combined clinical and endoscopic response occurred in 74% of caspofungin recipients and 63% of amphotericin B recipients 14 days after the completion of treatment; a favourable microbiological response occurred in 76% and 61% of patients. A favourable combined response rate of ≈90% and ≈60% occurred in the stratum of patients with oesophageal candidiasis who received caspofungin or amphotericin B in a third randomised, double-blind study (including patients with oropharyngeal or oesophageal candidiasis).
Retrospective analyses of oesophageal candidiasis trial data revealed that caspofungin 50 mg/day is effective in patients with oesophageal candidiasis who are refractory to fluconazole or are infected with Candida isolates that have reduced in vitro susceptibility to fluconazole, and is effective in eradicating the symptoms of oesophageal candidiasis in patients with HIV infection.
Caspofungin (70mg loading dose followed by 50 mg/day) had similar efficacy to amphotericin B (0.7–1.0 mg/kg/day in patients with neutropenia and 0.6–0.7 mg/kg/day in patients without neutropenia) in patients with invasive candidiasis. At the end of intravenous treatment, a favourable overall response occurred in 73.4% of caspofungin recipients and in 61.7% of amphotericin B recipients; caspofungin was shown to be noninferior to amphotericin B. Treatment failure occurred in 26.6% of caspofungin recipients and 38.3% of amphotericin B recipients. Similar proportions of caspofungin and amphotericin B recipients experienced relapse 6–8 weeks after the end of therapy (6.4% vs 7%) or died (34.2% vs 30.4%).
In a noncomparative study, salvage therapy with caspofungin (70mg loading dose followed by 50 mg/day) was effective in patients with invasive aspergillosis who were refractory to or did not tolerate standard antifungal therapy. A favourable response (complete plus partial response) occurred in 37 of 83 patients (45%). Analysis by the site of infection revealed a favourable response in 50%, 23% and 33% of patients with pulmonary aspergillosis, disseminated aspergillosis and single organ aspergillosis, respectively.
Tolerability
Caspofungin was generally well tolerated in clinical trials. In caspofungin recipients, the most commonly reported drug-related clinical adverse events included chills, fever, phlebitis/thrombophlebitis, tachycardia, nausea, vomiting, rash, abdominal pain, headache and diarrhoea (incidence ≤16%).
In comparative clinical trials, caspofungin had similar tolerability to fluconazole but was better tolerated than amphotericin B in patients with oesophageal or invasive candidiasis. Significantly fewer caspofungin than amphotericin B recipients reported drug-related clinical adverse events, specifically chills, fever, nausea or infusion-related adverse events. Caspofungin recipients were significantly less likely than amphotericin B recipients to discontinue therapy because of an adverse event. In addition, caspofungin recipients were significantly less likely than amphotericin B recipients to develop laboratory abnormalities or to discontinue treatment because of laboratory abnormalities. Significantly fewer caspofungin than amphotericin B recipients developed elevated blood urea nitrogen levels, decreased serum potassium levels/hypokalaemia, hypokalaemia requiring supplementation within 72 hours of onset, a nephrotoxic effect, decreased haemoglobin levels or increased serum creatinine levels.
With regards to potential drug interactions, coadministration of caspofungin and cyclosporin in healthy volunteers resulted in transient increases in alanine aminotransferase and aspartate aminotransferase levels. Patients receiving cyclosporin were generally excluded from clinical trials.
Dosage and Administration
Intravenous caspofungin is approved in the US for use in candidaemia; Candida-associated intra-abdominal abscess, peritonitis and pleural space infection; and oesophageal candidiasis. In the EU, intravenous caspofungin is approved for the treatment of invasive candidiasis in non-neutropenic patients. In both the US and the EU, intravenous caspofungin is indicated for use in patients with invasive aspergillosis who are refractory to or intolerant of other antifungal therapies.
Caspofungin should be administered by slow intravenous infusion over ≈1 hour. In invasive candidiasis (including candidaemia and other invasive Candida infections) and invasive aspergillosis, patients should receive a 70mg loading dose, followed by 50 mg/day thereafter. In oesophageal candidiasis, patients should receive caspofungin 50 mg/day (without a loading dose).
No dosage adjustment is needed in the elderly, in patients with renal dysfunction or in patients with mild hepatic impairment (Child-Pugh score 5–6), although in patients with moderate hepatic impairment (Child-Pugh score 7–9), the maintenance dosage of caspofungin should be reduced from 50 to 35 mg/day. No dose administration recommendations have been established for patients with severe hepatic impairment or in paediatric patients aged <18 years.
Concomitant administration of caspofungin and cyclosporin should be reserved for patients for whom the potential benefit outweighs the potential risk. When caspofungin is coadministered with tacrolimus, concentrations of the latter drug should be monitored and dosage adjustments made as necessary. An increased caspofungin dosage (70 mg/day) is recommended in patients receiving concomitant rifampicin and should be considered in patients concomitantly receiving inducers of drug clearance such as efavirenz, nevirapine, phenytoin, dexamethasone or carbamazepine.
Caspofungin should only be administered to pregnant women if the potential benefit justifies the potential risk to the fetus. US prescribing information recommends caution when administering caspofungin to breast-feeding women and EU prescribing information states that women receiving caspofungin should not breast feed.











Similar content being viewed by others
Notes
The use of tradenames is for product identification purposes only and does not imply endorsement.
References
Klepser ME. Antifungal resistance among Candida species. Pharmacotherapy 2001; 21 (8 Suppl. 2): 124S–32S
Stone EA, Fung HB, Kirschenbaum HL. Caspofungin: an echinocandin antifungal agent. Clin Ther 2002 Mar; 24(3): 351–77
Pacetti SA, Gelone SP. Caspofungin acetate for treatment of invasive fungal infections. Ann Pharmacother 2003 Jan; 37(1): 90–8
Groll AH, Walsh TJ. Caspofungin: pharmacology, safety and therapeutic potential in superficial and invasive fungal infections. Expert Opin Investig Drugs 2001 Aug; 10(8): 1545–58
Keating GM, Jarvis B. Caspofungin. Drugs 2001; 61(8): 1121–9; discussion 1130-1
Arikan S, Sancak B, Hascelik G. In vitro activity of caspofungin compared to that of amphotericin B, fluconazole, and itraconazole against Candida species [abstract no. PM144]. Int J Antimicrob Agents 2002 May; 19 Suppl. 1: S75
Cohen S, Carroll K. In vitro evaluation of pneumocandin activity against clinical isolates of yeasts [abstract no. C-166]. 99th General Meeting of the American Society for Microbiology; 1999 May 30–Jun 3; Chicago (IL)
Scott PM, Gerckens L, Lynch L, et al. Comparative in vitro susceptibility of clinical trial isolates to the echinocandin antifungal MK-991 [abstract no. J-5]. 38th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1998 Sep 24-27; San Diego (CA)
Sutton DA, Rinaldi MG, Fothergill AW. In vitro activity of the echinocandin caspofungin (MK-0991) against refractory clinical isolates of Candida and Aspergillus species [abstract no. J-113]. 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2001 Sep 22–25; Chicago (IL)
lattery AM, Scott Hicks P, Wilcox A, et al. In vitro susceptibility of clinical trial isolates of Aspergillus spp. to the glucan synthesis inhibitor caspofungin acetate (Cancidas™, MK-0991) [abstract and poster]. 40th International Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto
Ramesh MS, Baskaran I, Ganesan LT, et al. Postantifungal effect of older and newer antifungal agents on Aspergillus fumigatus and Candida albicans [abstract no. J-105]. 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2001 Sep 21–25; Chicago (IL)
Vazquez JA. In vitro evaluation of caspofungin acetate (Cancidas) against Candida glabrata: MICs, MFCs, time kill and synergy assays [abstract no. M-1509]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Geiss HK, Dilger S. The post-antifungal effect of caspofungin [abstract no. A-495]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Diekema DJ, Messer SA, Hollis RJ, et al. Antifungal activity of caspofungin and the new triazoles compared with itraconazole and amphotericin B against 462 recent clinical isolates of Aspergillus and other filamentous fungi [abstract no. M-1521]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
O'Shaughnessy EM, Peter J, Walsh TJ. In vitro additive and synergistic effect of two echinocandins, caspofungin and micafungin with voriconazole against Aspergillus fumigatus [abstract no. M-856]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Petraitis V, Petraitiene R, Kelaher A, et al. Antifungal activity and safety of caspofungin against experimental disseminated candidiasis in persistently nuetropenic rabbits [abstract no. M-188]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Bernard EM, Ishimaru T, Armstrong D. Low doses of the pneumocandin, L-743,872, are effective for prevention and treatment in an animal model of pulmonary aspergillosis [abstract no. F39]. 36th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1996 Sep 15–18; New Orleans (LA)
Douglas CM, Abruzzo G, Bowman JC, et al. Caspofungin alone or in combination with itraconazole reduces fungal burden in a neutropenic guinea pig model of disseminated aspergillosis [abstract no. M-1819]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Flattery AM, Bartizol K, Gill CJ, et al. Preclinical efficacy of MK-991 in combination with amphotericin B or fluconazole in mouse models of disseminated aspergillosis, candidiasis, and cryptococcisis [abstract no. J-61]. 38th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1998 Sep 24–27; San Diego (CA)
Oherov N, May GS, Albert NA, et al. Overexpression of Sbe2p, a golgi protein involved in cell wall formation confers resistance to caspofungin (CAS) in Saccharomyces cerevisiae [abstract no. J-1843]. 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2001 Sep 22–25; Chicago (IL)
Deresinski SC, Stevens DA. Caspofungin. Clin Infect Dis 2003 Jun 1; 36(11): 1445–57
Lomaestro BM. Caspofungin: an echinocandin antifungal for the treatment of invasive aspergillosis. Formulary 2001; 36(6): 427–36
Kontoyiannis DP, Lewis RE. Antifungal drug resistance of pathogenic fungi. Lancet 2002; 359(9312): 1135–44
Rex JH, Pfaller MA. Has antifungal susceptibility testing come of age? Clin Infect Dis 2002; 35(8): 982–9
National Committee for Clinical Laboratory Standards. Reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard (document M27-A). Wayne (PA): NCCLS, 1997
Espinel-Ingroff A. Antifungal susceptibility methods and their potential clinical relevance. Lab Med 2002; 33(8): 626–31
Bartizal K, Gill CJ, Abruzzo GK, et al. In vitro preclinical evaluation studies with the echinocandin antifungal MK-0991 (L-743,872). Antimicrob Agents Chemother 1997 Nov; 41(11): 2326–32
Barchiesi F, Schimizzi AM, Fothergill AW, et al. In vitro activity of the new echinocandin antifungal, MK-0991, against common and uncommon clinical isolates of Candida species. Eur J Clin Microbiol Infect Dis 1999; 18: 302–4
Vazquez JA, Lynch M, Boikov D, et al. In vitro activity of a new pneumocandin antifungal, L-743,872, against azole-susceptible and -resistant Candida species. Antimicrob Agents Chemother 1997 Jul; 41(7): 1612–4
Ernst EJ, Klepser ME, Ernst ME, et al. In vitro pharmacodynamic properties of MK-0991 determined by time-kill methods. Diagn Microbiol Infect Dis 1999; 33: 75–80
Bachmann SP, Patterson TF, López-Ribot JL. In vitro activity of caspofungin (MK-0991) against Candida albicans clinical isolates displaying different mechanisms of azole resistance. J Clin Microbiol 2002 Jun; 40(6): 2228–30
Espinel-Ingroff A. Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol 1998 Oct; 36(10): 2950–6
Krishnarao TV, Galgiani JN. Comparison of the in vitro activities of the echinocandin LY303366, the pneumocandin MK-0991, and fluconazole against Candida species and Cryptococcus neoformans. Antimicrob Agents Chemother 1997 Sep; 41(9): 1957–60
Marco F, Pfaller MA, Messer SA, et al. Activity of MK-0991 (L-743,872), a new echinocandin, compared with those of LY303366 and four other antifungal agents tested against blood stream isolates of Candida spp. Diagn Microbiol Infect Dis 1998; 31: 33–7
Pfaller MA, Diekema DJ, Messer SA, et al. In vitro activities of caspofungin compared with those of fluconazole and itraconazole against 3,959 clinical isolates of Candida spp., including 157 fluconazole-resistant isolates. Antimicrob Agents Chemother 2003 Mar; 47(3): 1068–71
Pfaller MA, Messer SA, Gee S, et al. In vitro susceptibilities of Candida dubliniensis isolates tested against the new triazole and echinocandin antifungal agents. J Clin Microbiol 1999 Mar; 37(3): 870–2
Nelson PW, Lozano-Chiu M, Rex JH. In vitro growth-inhibitory activity of pneumocandins L-733,560 and L-743,872 against putatively amphotericin B- and fluconazole-resistant Candida isolates: influence of assay conditions. J Med Vet Mycol 1997; 35: 285–7
Mora-Duarte J, Betts R, Rotstein C, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med 2002 Dec 19; 347(25): 2020–9
Villanueva A, Arathoon EG, Gotuzzo E, et al. A randomized double-blind study of caspofungin versus amphotericin for the treatment of candidal esophagitis. Clin Infect Dis 2001 Nov 1; 33(9): 1529–35
Villanueva A, Gotuzzo E, Arathoon EG, et al. A randomized double-blind study of caspofungin versus fluconazole for the treatment of esophageal candidiasis. Am J Med 2002 Sep; 113(4): 294–9
Ernst EJ, Klepser ME, Pfaller MA. Postantifungal effects of echinocandins, azole, and polyene antifungal agents against Candida albicans and Cryptococcus neoformans. Antimicrob Agents Chemother 2000 Apr; 44(4): 1108–11
Hossain MA, Reyes GH, Long LA, et al. Efficacy of caspofungin combined with amphotericin B against azole-resistant Candida albicans. J Antimicrob Chemother 2003 Jun; 51(6): 1427–9
Roling EE, Klepser ME, Wasson A, et al. Antifungal activities of fluconazole, caspofungin (MK0991), and anidulafungin (LY 303366) alone and in combination against Candida spp. and Crytococcus neoformans via time-kill methods. Diagn Microbiol Infect Dis 2002 May; 43(1): 13–7
Arikan S, Paetznick V, Rex JH. Comparative evaluation of disk diffusion with microdilution assay in susceptibility testing of caspofungin against Aspergillus and Fusarium isolates. Antimicrob Agents Chemother 2002 Sep; 46(9): 3084–7
Del Poeta M, Schell WA, Perfect JR. In vitro antifungal activity of pneumocandin L-743,872 against a variety of clinically important molds. Antimicrob Agents Chemother 1997 Aug; 41(8): 1835–6
Pfaller MA, Marco F, Messer SA, et al. In vitro activity of two echinocandin derivatives, LY303366 and MK-0991 (L-743,792), against clinical isolates of Aspergillus, Fusarium, Rhizopus, and other filamentous fungi. Diagn Microbiol Infect Dis 1998; 30: 251–5
del Carmen Serrano M, Valverde-Conde A, Chávez MM, et al. In vitro activity of voriconazole, itraconazole, caspofungin, anidulafungin (VER002, LY303366) and amphotericin B against aspergillus spp. Diagn Microbiol Infect Dis 2003 Feb; 45(2): 131–5
Arikan S, Lozano-Chiu M, Paetznick V, et al. In vitro susceptibility testing methods for caspofungin against Aspergillus and Fusarium isolates. Antimicrob Agents Chemother 2001 Jan; 45(1): 327–30
Bowman JC, Hicks PS, Kurtz MB, et al. The antifungal echinocandin caspofungin acetate kills growing cells of Aspergillus fumigatus in vitro. Antimicrob Agents Chemother 2002 Sep; 46(9): 3001–12
Arikan S, Lozano-Chiu M, Paetznick V, et al. In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother 2002 Jan; 46(1): 245–7
Shalit I, Shadkchan Y, Samra Z, et al. In vitro synergy of caspofungin and itraconazole against Aspergillus spp.: MIC versus minimal effective concentration end points. Antimicrob Agents Chemother 2003 Apr; 47(4): 1416–8
Manavathu EK, Alangaden GJ, Chandrasekar PH. Differential activity of triazoles in two-drug combinations with the echinocandin caspofungin against Aspergillus fumigatus. J Antimicrob Chemother 2003 Jun; 51(6): 1423–5
Perea S, Gonzalez G, Fothergill AW, et al. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of Aspergillus spp. Antimicrob Agents Chemother 2002 Sep; 46(9): 3039–41
Kontoyiannis DP, Lewis RE, Osherov N, et al. Combination of caspofungin with inhibitors of the calcineurin pathway attenuates growth in vitro in Aspergillus species. J Antimicrob Chemother 2003 Feb; 51(2): 313–6
Loeffler J, Stevens DA. Antifungal drug resistance. Clin Infect Dis 2003; 36 Suppl. 1: S31–41
Kurtz MB, Rex JH. Glucan synthase inhibitors as antifungal agents. Adv Protein Chem 2001; 56: 423–75
Schuetzer-Muehlbauer M, Willinger B, Krapf G, et al. The Candida albicans Cdr2p ATP-binding cassette (ABC) transporter confers resistance to caspofungin. Mol Microbiol 2003 Apr; 48(1): 225–35
Graybill JR, Najvar LK, Luther MF, et al. Treatment of murine disseminated candidiasis with L-743,872. Antimicrob Agents Chemother 1997 Aug; 41(8): 1775–7
Graybill JR, Bocanegra R, Luther M, et al. Treatment of murine Candida krusei or Candida glabrata infection with L-743,872. Antimicrob Agents Chemother 1997 Sep; 41(9): 1937–9
Ju JY, Polhamus C, Marr KA, et al. Efficacies of fluconazole, caspofungin, and amphotericin B in Candida glabrata-infected p47phox-/- knockout mice. Antimicrob Agents Chemother 2002 May; 46(5): 1240–5
Abruzzo GK, Gill CJ, Flattery AM, et al. Efficacy of the echinocandin caspofungin against disseminated aspergillosis and candidiasis in cyclophosphamide-induced immunosuppressed mice. Antimicrob Agents Chemother 2000 Sep; 44(9): 2310–8
Abruzzo GK, Flattery AM, Gill CJ, et al. Evaluation of the echinocandin antifungal MK-0991 (L-743,872): efficacies in mouse models of disseminated aspergillosis, candidiasis, and cryptococcosis. Antimicrob Agents Chemother 1997 Nov; 41(11): 2333–8
Graybill JR, Bocanegra R, Najvar LK, et al. Addition of caspofungin to fluconazole does not improve outcome in murine candidiasis. Antimicrob Agents Chemother 2003 Jul; 47(7): 2373–5
Kirkpatrick WR, Perea S, Coco BJ, et al. Efficacy of caspofungin alone and in combination with voriconazole in a guinea pig model of invasive aspergillosis. Antimicrob Agents Chemother 2002 Aug; 46(8): 2564–8
Bowman JC, Abruzzo GK, Anderson JW, et al. Quantitative PCR assay to measure Aspergillus fumigatus burden in a murine model of disseminated aspergillosis: demonstration of efficacy of caspofungin acetate. Antimicrob Agents Chemother 2001 Dec; 45(12): 3474–81
Petraitiene R, Petraitis V, Groll AH, et al. Antifungal efficacy of caspofungin (MK-0991) in experimental pulmonary aspergillosis in persistently neutropenic rabbits: pharmacokinetics, drug disposition, and relationship to galactomannan antigenemia. Antimicrob Agents Chemother 2002 Jan; 46(1): 12–23
Powles MA, Liberator P, Anderson J, et al. Efficacy of MK-991 (L-743,872), a semisynthetic pneumocandin, in murine models of Pneumocystis carinii. Antimicrob Agents Chemother 1998 Aug; 42(8): 1985–9
Merck & Co. Cancidas® (caspofungin acetate) for injection: prescribing information [online]. Available from URL: http://www.cancidas.com [Accessed 2003 Jun 13]
Stone JA, Ballow CH, Holland S, et al. Single dose caspofungin pharmacokinetics in healthy elderly subjects [abstract and poster]. 40th International Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto
Stone J, Holland S, Li S, et al. Effect of hepatic insufficiency on the pharmacokinetics of caspofungin [abstract no. A-14]. 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2001 Sep 22–25; Chicago (IL)
Stone JA, McCrea J, Wickersham P, et al. A phase I study of caspofungin evaluating the potential for drug interactions with itraconazole, the effect of gender and the use of a loading dose regimen [abstract and poster]. 40th International Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto
Stone J, Holland S, Wickersham P, et al. Drug interactions between caspofungin and tacrolimus [abstract no. A-13]. 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 2001 Sep 22–25; Chicago (IL)
Stone JA, Holland SD, Wickersham PJ, et al. Single- and multiple-dose pharmacokinetics of caspofungin in healthy men. Antimicrob Agents Chemother 2002 Mar; 46(3): 739–45
Hajdu R, Thompson R, Sundelof JG, et al. Preliminary animal pharmacokinetics of the parenteral antifungal agent MK-0991 (L-743,872). Antimicrob Agents Chemother 1997 Nov; 41(11): 2339–44
Balani SK, Xu X, Arison BH, et al. Metabolites of caspofungin acetate, a potent antifungal agent, in human plasma and urine. Drug Metab Dispos 2000; 28(11): 1274–8
Maertens J, Raad I, Petrikkos G, et al. Update of the multicenter noncomparative study of caspofungin (CAS) in adults with invasive aspergillosis (IA) refractory (R) or intolerant (I) to other antifungal agents: analysis of 90 patients [abstract no. M-868]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Maertens J, Raad I, Sable CA, et al. Multicenter, noncomparative study to evaluate safety and efficacy of caspofungin (CAS) in adults with invasive aspergillosis (IA) refractory (R) or intolerant (I) to amphotericin B (AMB), AMB lipid formulations (lipid AMB), or azoles [abstract and poster]. 40th International Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto
Arathoon EG, Gotuzzo E, Noriega LM, et al. Randomized, double-blind, multicenter study of caspofungin versus amphotericin B for treatment of oropharyngeal and esophageal candidiases. Antimicrob Agents Chemother 2002 Feb; 46(2): 451–7
Kartsonis N, DiNubile MJ, Bartizal K, et al. Efficacy of caspofungin in the treatment of esophageal candidiasis resistant to fluconazole. J Acquir Immune Defic Syndr 2002 Oct 1; 31(2): 183–7
DiNubile MJ, Lupinacci RJ, Berman RS, et al. Response and relapse rates of candidal esophagitis in HIV-infected patients treated with caspofungin. AIDS Res Hum Retroviruses 2002 Sep 1; 18(13): 903–8
Data on file, Merck & Co., Inc., 2003
Merck Sharp and Dohme Limited. Caspofungin MSD: summary of product characteristics [online]. Available from URL: http://emc.medicines.org.uk [Accessed 2003 Aug 1]
Chiou CC, Groll AH, Walsh TJ. New drugs and novel targets for treatment of invasive fungal infections in patients with cancer. Oncologist 2000; 5(2): 120–35
Maschmeyer G. New antifungal agents — treatment standards are beginning to grow old. J Antimicrob Chemother 2002 Feb; 49(2): 239–41
Rex JH, Walsh TJ, Sobel JD, et al. Practice guidelines for the treatment of candidiasis. Clin Infect Dis 2000 Apr; 30(4): 662–78
Stevens DA, Kan VL, Judson MA, et al. Practice guidelines for diseases caused by Aspergillus. Clin Infect Dis 2000; 30: 696–709
Vazquez J. Invasive oesophageal candidiasis: current and developing treatment options. Drugs 2003; 63(10): 971–89
Ostrosky-Zeichner L, Rex JH, Bennett J, et al. Deeply invasive candidiasis. Infect Dis Clin N Am 2002; 16(4): 821–35
Denning DW, Kibbler CC, Barnes RA. British Society for Medical Mycology proposed standards of care for patients with invasive fungal infections. Lancet Infect Dis 2003 Apr; 3(4): 230–40
Rex JH, Pfaller MA, Walsh J, et al. Antifungal susceptibility testing: practical aspects and current challenges. Clin Microbiol Rev 2001; 14(4): 643–58
Pfaller MA, Messer SA, Mills K, et al. Evaluation of Etest method for determining caspofungin (MK-0991) susceptibilities of 726 clinical isolates of Candida species. J Clin Microbiol 2001 Dec; 39(12): 4387–9
Chryssanthou E, Cuenca-Estrella M. Comparison of the Antifungal Susceptibility Testing Subcommittee of the European Committee on Antibiotic Susceptibility Testing proposed standard and the E-test with the NCCLS broth microdilution method for voriconazole and caspofungin susceptibility testing of yeast species. J Clin Microbiol 2002 Oct; 40(10): 3841–4
Espinel-Ingroff A. Evaluation of broth microdilution testing parameters and agar diffusion Etest procedure for testing susceptibilities of Aspergillus spp. to caspofungin acetate (MK-0991). J Clin Microbiol 2003 Jan; 41(1): 403–9
Laverdiere M, Restieri C, Habel F. Evaluation of the in vitro activity of caspofungin against bloodstream isolates of Candida species from cancer patients: comparison of Etest and NCCLS reference methods. Int J Antimicrob Agents 2002 Dec; 20(6): 468–71
Rogers TR. Optimal use of existing and new antifungal drugs. Curr Opin Crit Care 2001 Aug; 7(4): 238–41
Kontoyiannis DP. A clinical perspective for the management of invasive fungal infections: focus on IDSA guidelines. Pharmacotherapy 2001 Aug; 21 (8 Pt 2): 175S–87S
Walsh TJ. Echinocandins: an advance in the primary treatment of invasive candidiasis. N Engl J Med 2002 Dec 19; 347(25): 2070–2
De Pauw BE, Donnelly JP, Verweij PE, et al. Current management of fungal infections in immunocompromised patients and polyene lipid complexes for treatment of invasive fungal infection. J Infect Dis Antimicrob Agents 1998; 15: 85–96
Patterson TF. Recent developments in the diagnosis and treatment of invasive aspergillosis. Rev Med Microbiol 2001; 12 Suppl. 1: S37–42
Reichenberger F, Habicht JM, Gratwohl A, et al. Diagnosis and treatment of invasive pulmonary aspergillosis in neutropenic patients. Eur Respir J 2002; 19(4): 743–55
Harari S. Current strategies in the treatment of invasive Aspergillus infections in immunocompromised patients. Drugs 1999 Oct; 58: 621–31
Perea S, Patterson TF. Invasive Aspergillus infections in hematologic malignancy patients. Semin Respir Infect 2002 Jun; 17(2): 99–105
Lum LR, Turco TF, Leone J. Combination therapy with caspofungin and amphotericin B lipid complex [letter]. Am J Health Syst Pharm 2002 Jan 1; 59(1): 80–1
Aliff TB, Maslak PG, Jurcic JG, et al. Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer 2003 Feb 15; 97(4): 1025–32
Kontoyiannis DP, Hachem R, Lewis RE, et al. Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer 2003 Jul 15; 98(2): 292–9
Thiébaut A, Antal D, Breysse MC, et al. Refractory invasive fungal infections in patients (pts) with hematologic malignancies: combination of new antifungal agents (voriconazole or caspofungin) with amphotericin B [abstract no. M-859]. 42nd Interscience Conference on Antimicrobial Agents and Chemotherapy; 2002 Sep 27–30; San Diego (CA)
Kontoyiannis DP, Bodey GP. Invasive aspergillosis in 2002: an update. Eur J Clin Microbiol Infect Dis 2002; 21(3): 161–72
Muijsers RBR, Goa KL, Scott LJ. Voriconazole in the treatment of invasive aspergillosis. Drugs 2002; 62(18): 2655–64
Pfizer Inc. Prescribing information: VFEND tablets (voriconazole) and VFEND IV (voriconazole) for injection [online]. Available from URL: http://www.pfizer.com [Accessed 2003 Jun 24]
European Agency for the Evaluation of Medicinal Products. Summary of product characteristics: voriconazole [online]. Available from URL: http://www.emea.eu.int [Accessed 2003 Jun 24]
Fujisawa Pharmaceutical Co., Ltd.. Fujisawa launches the candin antifungal agent, Funguard® for Infusion [media release]. Available from URL: http://www.fujisawa.co.jp [Accessed 2003 Jun 30]
Vicuron Pharmaceuticals. Vicuron submits New Drug Application for anidulafungin to FDA [media release]. Available from URL: http://www.vicuron.com [Accessed 2003 Jul 31]
Hebart H, Bokemeyer C, Loffler J, et al. Management of invasive fungal infections in oncological patients. Onkologie 1999 Jun; 22: 192–7
Vazquez JA. Options for the management of mucosal candidiasis in patients with AIDS and HIV infection. Pharmacotherapy 1999 Jan; 19: 76-87
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: B.E. de Pauw, University Medical Center St Radboud, Nijmegen, The Netherlands; A. Espinel-Ingroff, Medical College of Virginia, Virginia Commonwealth University, Richmond, Virginia, USA; H.B. Fung, Critical Care Center, Veterans Affairs Medical Center, Bronx, New York, USA; A.H. Groll, Wilhelms-University Medical Center, Muenster, Germany; M.E. Klepser, Borgess Medical Center, Ferris State University, Kalamazoo, Michigan, USA; J. Maertens, Department of Haematology, University Hospital Gasthuisberg, Leuven, Belgium; V.A. Morrison, Section of Hematology/Oncology, Veterans Affairs Medical Center, Minneapolis, Minnesota, USA; M.A. Pfaller, Department of Pathology, University of Iowa, Iowa City, Iowa, USA; J.A. Vazquez, Division of Infectious Diseases, Wayne State University School of Medicine, Detroit, Michigan, USA.
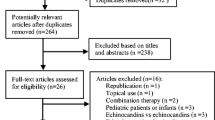
Data Selection
Sources: Medical literature published in any language since 1980 on caspofungin, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline and EMBASE search terms were ‘caspofungin’. AdisBase search terms were ‘caspofungin’ or ‘MK 099’ or ‘MK 991’ or ‘L-743872’. Searches were last updated 18 August 2003.
Selection: Studies in patients with oesophageal candidiasis, invasive candidiasis or invasive aspergillosis who received caspofungin. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: caspofungin, invasive aspergillosis, oesophageal candidiasis, invasive candidiasis, pharmacodynamics, pharmacokinetics, therapeutic use.
Rights and permissions
About this article
Cite this article
Keating, G.M., Figgitt, D.P. Caspofungin. Drugs 63, 2235–2263 (2003). https://doi.org/10.2165/00003495-200363200-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200363200-00008