- 1Department of Global Health, University of Washington, Seattle, WA, United States
- 2Public Health—Seattle and King County, Seattle, WA, United States
- 3Office of Communicable Disease Epidemiology, Washington State Department of Health, Seattle, WA, United States
- 4Department of Health Services, University of Washington, Seattle, WA, United States
The COVID-19 pandemic continues to expand globally, requiring massive public health responses from national and local governments. These bodies have taken heterogeneous approaches to their responses, including when and how to introduce and enforce evidence-based interventions—such as social distancing, hand-washing, personal protective equipment (PPE), and testing. In this commentary, we reflect on opportunities for implementation science to contribute meaningfully to the COVID-19 pandemic response. We reflect backwards on missed opportunities in emergency preparedness planning, using the example of PPE stockpiling and supply management; this planning could have been strengthened through process mapping with consensus-building, microplanning with simulation, and stakeholder engagement. We propose current opportunities for action, focusing on enhancing the adoption, fidelity, and sustainment of hand washing and social distancing; we can combine qualitative data, policy analysis, and dissemination science to inform agile and rapid adjustment to social marketing strategies to enhance their penetration. We look to future opportunities to enhance the integration of new evidence in decision-making, focusing on serologic and virologic testing systems; we can leverage simulation and other systems engineering modeling to identify ideal system structures. Finally, we discuss the ways in which the COVID-19 pandemic challenges implementation science to become more rapid, rigorous, and nimble in its approach, and integrate with public health practice. In summary, we articulate the ways in which implementation science can inform, and be informed by, the COVID-19 pandemic, looking backwards, proposing actions for the moment, and approaches for the future.
Contributions to the Literature
• The COVID-19 pandemic response has illuminated gaps in emergency preparedness planning that could be addressed by implementation scientists working in coordination with public health practitioners.
• Classical implementation science tools and measures can be operationalized within the context of the COVID-19 pandemic, and at each stage of the pandemic. Doing so empowers implementation scientists to apply their skillsets toward optimizing uptake of evidence-based interventions such as such as social distancing, hand washing, and personal protective equipment.
• To be more responsive to public health emergencies, implementation science as a discipline must evolve to be more rapid, nimble, and policy-oriented in its approaches.
Introduction
COVID-19 has emerged in early 2020 as a pandemic, marked by a classical exponential growth curve and global spread. National and local governments have taken heterogeneous approaches to curbing disease spread, relying on staggered and incomplete implementation of evidence-based public health behavioral prevention interventions, such as hand-washing and social distancing. State and local public health response efforts have focused on testing populations of public health significance, case and contact investigation, and infection prevention. Medical response to this novel virus has relied on limited supplies of personal protective equipment (PPE) for providers, ventilation assistance for severe cases, and testing. Development and trials of new interventions—including chemoprophylaxis and treatments, vaccines, and serologic tests—are underway.
Implementation science (IS) can be used to expand effective uptake of evidence-based interventions, such as hand washing, PPE use, ventilation, and social distancing. While epidemiology is the foundation of a robust pandemic response, IS methods can be used to understand how to protect historically excluded populations, rapidly engender necessary behavior change, and communicate data back to decision makers in a format that is actionable. IS relies on a broad toolkit from multiple disciplines including social science and mixed-methods, and is a necessary complement to traditional epidemiology. Domestically, IS has drawn heavily on frameworks, methods, and tools from behavioral science; in the global health context, IS draws on a broader array of frameworks, methods and tools (1). At the core of IS is the pursuit of effective and equitable collaborations and balancing systematization with system agility. In this Perspective piece, we articulate ways in which IS can inform, and be informed by, the COVID-19 pandemic.
Operationalizing is for COVID-19
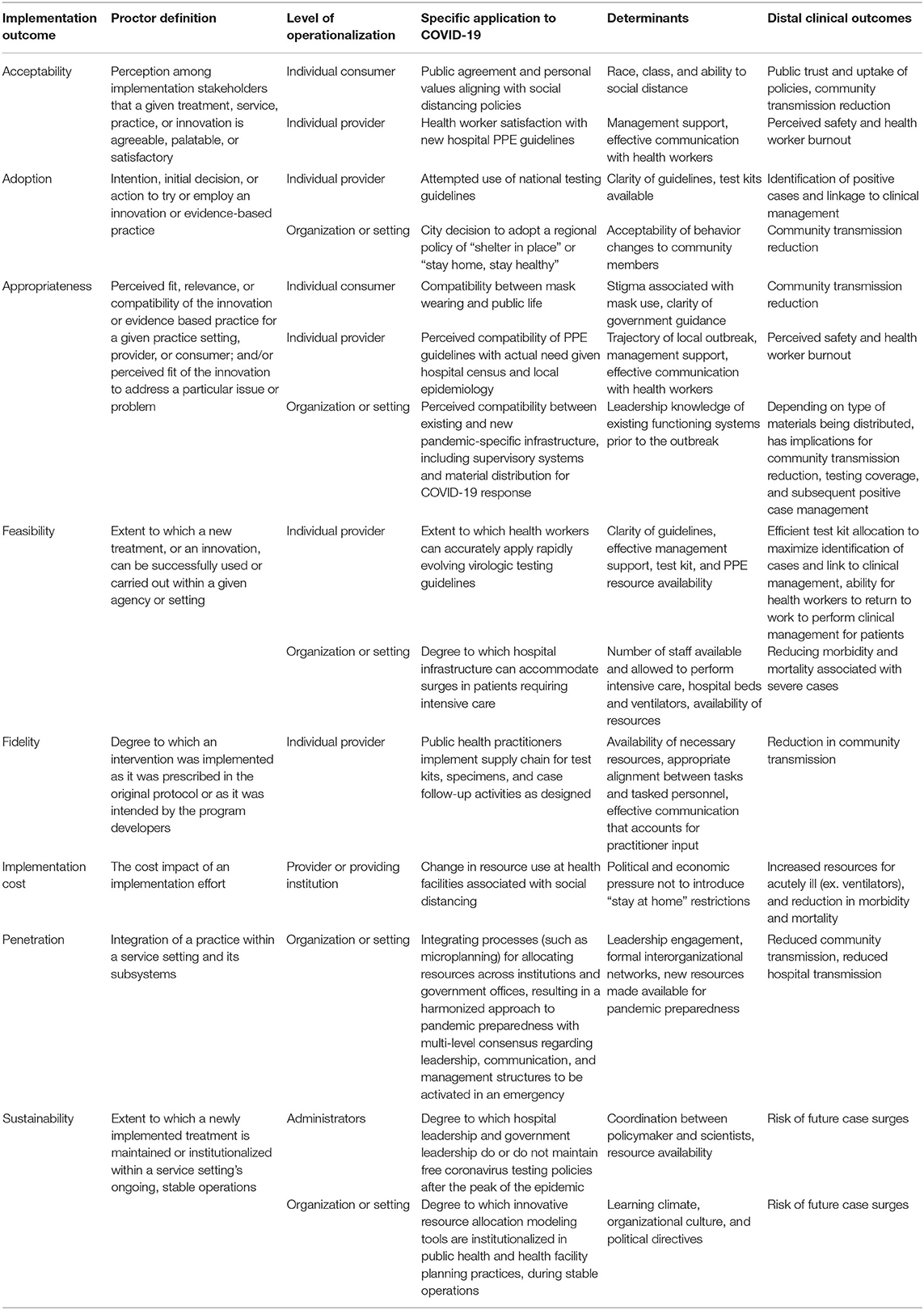
IS focuses on characterizing and enhancing the acceptability, adoption, appropriateness, feasibility, fidelity, cost, penetration, and sustainability of evidence-based interventions in distinct settings (2). Within the context of COVID-19, we propose operational definitions of these outcomes at the individual, provider (clinical providers and public health workers broadly), and organizational levels, identify determinants (barriers and facilitators) to implementation, and distal clinical outcomes (Table 1). We further highlight current and anticipated areas of IS inquiry, relevant implementation outcomes, pragmatic methods, and implementation strategies that may be primed to activate targeted outcomes (Table 2) (26). Finally, we describe how the lessons from the COVID-19 pandemic can inform the discipline of IS to become a more nimble, rapid, and agile (27). In the sections that follow, we highlight specific selected examples in the text; however, Tables 1,2 provide rich and comprehensive examinations of the application of IS to COVID-19.
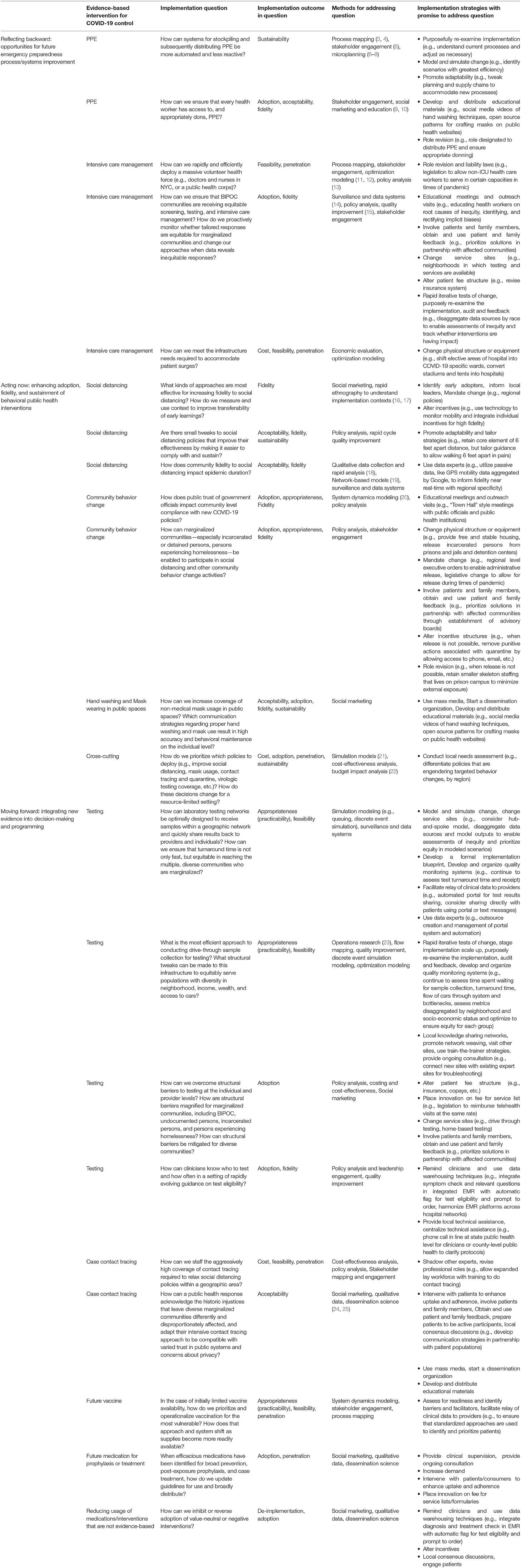
Table 2. Key implementation questions, outcomes, methods, and strategies for evidence-based COVID-19 interventions, at different stages of the pandemic.
Reflecting Backward: Role of is in Planning for Emergency Preparedness Pre-Pandemic
IS can contribute to pandemic preparedness by improving both robustness and agility of systems, drawing from contributing and relevant disciplines such as industrial engineering, business, political science, and more (3, 4, 27). We suggest that robust systems employ expertise and tools that are fit for purpose, while agile systems are built to be adaptable and flexible in quickly changing conditions. IS provides a systems approach to identify and test implementation strategies that can be used to enhance the robustness and agility of systems through the rapid deployment of evidence-based interventions, when available.
Process maps can be used to outline how human and material resources may be distributed under a variety of scenarios. Process mapping methods originated in the manufacturing industry as a quality improvement tool to improve existing processes, or as a formative pre-implementation planning tool (3, 28). To ensure that maps are representative and operational, consensus on the process maps should be reached in advance and account for the perspectives of multi-level stakeholders with responsibilities ranging from planning to front-line service delivery. In this context, microplanning together with extensive stakeholder mapping can establish avenues for deploying evidence-based interventions, even in the absence of specific interventions themselves. These strategies will inevitably require adaptation to fit the context of the disease and necessitated disease management, but will ideally require revision rather than reinvention, saving valuable time during a pandemic.
For example, public health departments in the United States (U.S.) follow the Incident Command System, part of the National Incident Management System, and have developed emergency preparedness systems and policies for how human and material resources—such as PPE, medical workers, case investigators, data collection and reporting staff—are intended to be distributed in times of emergency (29). However, the early COVID-19 response in the U.S. illuminated challenges in the distribution of key resources, such as PPE. Integrated within process mapping development and stakeholder validation processes, implementation scientists can collaborate with public health planners or emergency preparedness personnel to apply simulation and microplanning tools to determine how much PPE would be required under a variety of epidemiologic scenarios and operational constraints affecting their availability (6, 8). Microplans are localized and detailed assessments and plans for implementation, including the resources, timing, and personnel involved (7, 30). Often referred to as “bottom-up planning,” microplans might, for example, detail PPE requirements and constraints across a variety of federal funding scenarios, reproductive rates, and supply chain structures. Newly developed microplans can, as a result, provide a data-informed and tiered planning protocol where stockpiles are iteratively adjusted as human resources fluctuate or supply chains are compromised due to changes in distribution channels (Table 2). Such an approach requires redefining concepts of “lean” implementation at present to consider future wastage of time, a vital resource during a pandemic. Additional examples of how IS might be applied to planning for emergency preparedness are reflected in Table 2.
Acting Now: Enhancing Adoption, Fidelity, and Sustainment of Hand Washing and Social Distancing
In the absence of widespread testing, bending the COVID-19 curve is predicated on broad uptake of social distancing and individual-level hygiene behaviors. Public health departments and medical institutions throughout the world have invested in health communication and social mobilization to communicate the importance of these activities with communities. Linking qualitative data (including data from the private sector, such as Google searches, YouTube views, and GPS mobility), policy analysis, and dissemination science can produce real-time information regarding public reactions to government and employer-issued guidance, which can be used to understand what social marketing strategies penetrate effectively with target populations. These insights can inform quick revision of social marketing strategies and policy design in other affected jurisdictions with compatible implementation climates. For example, lessons learned from early messaging might be transferable between settings with comparable population demographics, health care infrastructure, and public health departments to increase message penetration earlier in an epidemic. Similarly, incorporating rapid feedback from stakeholders is necessary for ensuring that programs perform as expected (Table 2). Rapid feedback from community members can be collated during an outbreak using social media, crowdsourced innovations, or media monitoring. Rapid feedback from clinical or public health responders can be collated by appointing an information disseminator, whose primary responsibility is to attend daily planning/debriefing meetings to document what activities are working well, and which require adaptation or abandonment. These lessons learned can then be disseminated to community members and other health jurisdictions periodically.
Different populations have differential ability to adopt and sustain social distancing interventions; immediate IS actions must explicitly take an equity lens (31). For example, social distancing is not feasible for incarcerated individuals or undocumented individuals in detention (32). Orders to “stay home, stay healthy” are not possible for individuals experiencing homelessness (33). COVID-19 has disproportionately affected Black, indigenous, and persons of color (BIPOC) communities; guidelines to seek testing and medical management are differentially experienced by communities of color who may have poorer access to services and higher risk of poor health outcomes from COVID-19 due to historic and current injustices, individual and structural racism, environmental racism, and bias in the quality of health services delivered (34). Employing IS methods and strategies that illuminate and combat inequity—such as disaggregating surveillance data by race, changing physical structures to provide housing and to release detained or incarcerated persons, altering incentive structures to make testing and medical coverage independent of citizenship, engaging communities in identifying and testing solutions—will be essential for immediate impact on equity (Table 2). However, mitigating the impacts of inequity at an individual and organizational level is insufficient; a simultaneous approach to address upstream drivers of inequity and dismantle oppressive systems at the structural level is essential for future public health prevention. Additional examples of how IS can be utilized now to curb epidemic spread are presented in Table 2.
A key implementation determinant influencing adoption, fidelity, and cost of COVID-19 control strategies is ineffective communication channels, resulting in protocols that are interpreted differently across settings and unnecessary implementation delays. For example, a large number of health workers have been infected, resulting in a health workforce that is stretched thinly in many areas (35, 36). Yet, in the U.S., confusion regarding when health workers can return to work after symptom resolution has exacerbated this problem due to existence of multiple protocols (37). Delays clarifying return to work protocols at one point appeared tied to faulty supply of testing kits, rather than evidence (Table 1) (38).
Moving Forward: Integrating New Evidence Into Decision-Making
Even in the absence of an evidence-based intervention, IS can guide evidence-based decision-making as data become available. This means having systems that help governments and health facilities incorporate evidence agilely: key attributes include strengthening stakeholder networks with clear communication channels, social mobilization mechanisms that can be quickly activated, and microplanning tools to rapidly guide resource allocation. As we transition to recovery and reflection from the pandemic, key implementation outcomes to consider include penetration and sustainability (Table 1). For penetration, we ask whether best practices of microplanning and stakeholder engagement have been integrated into routine pandemic preparedness in all countries and health jurisdictions? For sustainability, we evaluate whether governments have established necessary policies and programs needed to support these activities longer-term, throughout recovery, and evolving back into preparedness. Key implementation science questions related to enhancing these implementation outcomes applied to current and future evidence based interventions are highlighted in Table 2.
Advanced use of modeling aimed at pragmatic decision-making can inform efficient resource allocation—human resources, tests, PPE, ventilators—when they become available, avoiding bottlenecks in distribution seen with volunteer medical personnel in New York City (39). Sophisticated mathematical models ideally suited to answer epidemiologic spread questions have already been useful in informing decision-making; these complex models are resource-intensive to create and are best suited to scenarios where existing models can be adapted, or a new model can inform many “what if” scenarios (40–43). Sophisticated mathematical models have been crucial in informing how conditions would need to be modified to not overload an existing health system, which has influenced state-level policies on social distancing and shelter in place policy timing (41). Additionally, this modeling has been translated into accessible infographics to reinforce the immediate urgency of fidelity to social distancing to curb spread.
In contrast, several types of systems engineering models may be less resource intensive to create and can be useful to inform local decision-making (Table 2). For example, as serologic tests are developed and virologic testing capacity expands, there are questions of where to situate central laboratories within hub-and-spoke models or how to arrange distribution of rapid point-of-care tests from a centralized point. For example, queuing modeling has been used to prospectively plan for resource allocation for other diseases, such as HIV (21, 44). As an effective vaccine becomes available, advanced use of these models can accelerate efficient distribution by prioritizing certain values—such as maximizing equity, or minimizing costs—and can compare a range of scenarios for decision-makers. These modeling tools can be developed now, as new evidence-based interventions are either created or scaled up.
Learning About Implementation During COVID-19
IS is an emerging discipline with rapidly evolving methods for measuring outcomes and determinants, testing strategies, and assessing context; as with any emerging discipline, it takes time to develop both rigorous and pragmatic methods. However, time invested in measurement calibration can contribute to a further delay in getting “what works,” evidence-based interventions, to populations who need them. The COVID-19 pandemic makes a critical case for rapid, rigorous, nimble, and pragmatic IS.
The pandemic response highlights two lacunae in IS foci. First, an inattention to supply chain and logistics. IS conducted in low-and-middle income countries often addresses resource supply and logistics because they are acutely and chronically observed as implementation determinants (45, 46). Yet, they are relatively absent from IS literature in high-income countries. A second gap is inattention to politics as an implementation barrier or facilitator. While external policies and incentives are addressed in many established frameworks and checklists, implementation scientists do not often incorporate political science perspectives or theories within their work (47, 48). Many of the suggestions presented in this perspective depend upon and assume government cooperation with health departments and accountability to scientific leadership. The COVID-19 pandemic has made it abundantly clear that implementation scientists can no longer overlook the importance of politics as a major implementation determinant.
In the immediate future, implementation scientists can be more “real time” with their questions and findings by using routinely available data, rather than primary data; for example, aggregated trends in Google mobility data as a proxy for fidelity to social distancing. Implementation scientists can utilize non-experimental designs for robust impact evaluation—such as regression discontinuity (including interrupted time series) and difference in differences—without additional dedicated research funding. In the coming years, IS as a discipline can focus on improving the rigor and rapidity of validated measures—including simple scales for assessing implementation outcomes, determinants, and context. These measures should be relevant across geographic and sociocultural settings. Finally, IS will benefit from more purposeful integration within public health departments and health organizations, not exclusively within academic organizations.
Conclusions
Many of the challenges hindering effective COVID-19 response to date have been driven by operational, logistical, and social factors. IS, public health, medical, and governmental communities can work together to inform a stronger response to the COVID-19 pandemic. Missed opportunities in the past illuminate opportunities for future revisions in how we approach emergency preparedness planning. Simultaneously, this pandemic challenges implementation scientists to continue to endeavor to become more rapid and nimble in addressing the public health emergencies of the future.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
AW and AM conceptualized and wrote the first draft of the manuscript. EK, LN, and BW reviewed and revised the manuscript. All authors reviewed and approved the final version of this manuscript.
Funding
AW was supported by K01MH121124.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We acknowledge the Implementation Science Program and the Global WACh center at the University of Washington for their support. We thank the health care providers, public health practitioners, and implementers for their extraordinary work during the COVID-19 pandemic. We thank Marie-Claire Gwayi-Chore and Sofia Nelson for their insights and resources on strategies for more equitably serving communities of color and persons incarcerated in jails and prisons.
References
1. Theobald S, Brandes N, Gyapong M, El-Saharty S, Proctor E, Diaz T, et al. Implementation research: new imperatives and opportunities in global health. Lancet. (2018) 392:2214–28. doi: 10.1016/S0140-6736(18)32205-0
2. Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, research agenda. Adm Policy Mental Health. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
3. McCreight MS, Gilmartin HM, Leonard CA, Mayberry AL, Kelley LR, Lippmann BK, et al. Practical use of process mapping to guide implementation of a care coordination program for rural Veterans. J Gen Intern Med. (2019) 34:67–74. doi: 10.1007/s11606-019-04968-x
4. Nensi A, Simpson A, Kives S, Lei R, D'Souza J, Robertson D. Utilizing lean methodology to optimize operating room efficiency: a multidisciplinary process mapping exercise. Am J Med Qual. (2020) 35:91. doi: 10.1177/1062860619889884
5. Goodman MS, Sanders Thompson VL. The science of stakeholder engagement in research: classification, implementation, and evaluation. Transl Behav Med. (2017) 7:486–91. doi: 10.1007/s13142-017-0495-z
6. Bhattacharjee P, Musyoki H, Prakash R, Malaba S, Dallabetta G, Wheeler T, et al. Micro-planning at scale with key populations in Kenya: optimising peer educator ratios for programme outreach and HIV/STI service utilisation. PLoS One. (2018) 13:e0205056. doi: 10.1371/journal.pone.0205056
7. WHO. Microplanning for Immunization Service Delivery Using the Reaching Every District (RED) Strategy. Geneva: World Health Organization (2009).
8. Umeh GC, Madubu DM, Korir C, Loveday N, Ishaku S, Iyal H, et al. Micro-planning for immunization in Kaduna state, Nigeria: lessons learnt, 2017. Vaccine. (2018) 36:7361–8. doi: 10.1016/j.vaccine.2018.10.020
9. Cugelman B, Thelwall M, Dawes P. Online interventions for social marketing health behavior change campaigns: a meta-analysis of psychological architectures and adherence factors. J Med Internet Res. (2011) 13:e17. doi: 10.2196/jmir.1367
10. Sweat MD, Yeh T, Kennedy C, O'Reilly K, Armstrong K, Fonner V. Condom social marketing effects in low-and middle-income countries: a systematic review update, 1990 to 2019. Am J Health Promot. (2020) 34:91–5. doi: 10.1177/0890117119864921
11. Alistar SS, Long EF, Brandeau ML, Beck EJ. HIV epidemic control-a model for optimal allocation of prevention and treatment resources. Health Care Manage Sci. (2014) 17:162–81. doi: 10.1007/s10729-013-9240-4
12. Omar, E.-R., Garaix T, Augusto V, Xie X. A stochastic optimization model for shift scheduling in emergency departments. Health Care Manage Sci. (2015) 18:289–302. doi: 10.1007/s10729-014-9300-4
13. Engelman A, Case B, Meeks L, Fetters MD. Conducting health policy analysis in primary care research: turning clinical ideas into action. Fam Med Commun Health. (2019) 7:e000076. doi: 10.1136/fmch-2018-000076
14. Wagenaar BH, Sherr K, Fernandes Q, Wagenaar AC. Using routine health information systems for well-designed health evaluations in low-and middle-income countries. Health Policy Plann. (2016) 31:129–35. doi: 10.1093/heapol/czv029
16. Ackerman S, Gleason N, Gonzales R. Using rapid ethnography to support the design and implementation of health information technologies. Stud Health Technol Inform. (2015) 215:14–27. doi: 10.3233/978-1-61499-560-9-14
17. Ackerman SL, Sarkar U, Tieu L, Handley MA, Schillinger D, Hahn K, et al. Meaningful use in the safety net: a rapid ethnography of patient portal implementation at five community health centers in California. J Am Med Inform Assoc. (2017) 24:903–12. doi: 10.1093/jamia/ocx015
18. Brown-Johnson C, Shaw JG, Safaeinili N, Chan GK, Mahoney M, Asch S, et al. Role definition is key-R apid qualitative ethnography findings from a team-based primary care transformation. Learn Health Syst. (2019) 3:e10188. doi: 10.1002/lrh2.10188
19. Enns EA, Brandeau ML. Link removal for the control of stochastically evolving epidemics over networks: a comparison of approaches. J Theor Biol. (2015) 371:154–65. doi: 10.1016/j.jtbi.2015.02.005
20. Zimmerman L, Lounsbury DW, Rosen CS, Kimerling R, Trafton JA, Lindley SE. Participatory system dynamics modeling: increasing stakeholder engagement and precision to improve implementation planning in systems. Adm Policy Mental Health. (2016) 43:834–49. doi: 10.1007/s10488-016-0754-1
21. Gonsalves GS, Paltiel AD, Cleary PD, Gill MJ, Kitahata MM, Rebeiro PF, et al. A flow-based model of the HIV care continuum in the United States. J Acquir Immune Defic Syndr. (2017) 75:548–53. doi: 10.1097/QAI.0000000000001429
22. Cherutich P, Farquhar C, Wamuti B, Otieno FA, Mutiti PM, Macharia P, et al. HIV partner services in Kenya: a cost and budget impact analysis study. BMC Health Services Res. (2018) 18:1–11. doi: 10.1186/s12913-018-3530-y
23. Monks T. Operational research as implementation science: definitions, challenges and research priorities. Implement Sci. (2015) 11:81. doi: 10.1186/s13012-016-0444-0
24. Pollack KM, Schmid TL, Wilson AL, Schulman E. Advancing translation and dissemination research and practice through the physical activity policy research network plus. Environ Behav. (2016) 48:266–72. doi: 10.1177/0013916515616990
25. Purtle J, Brownson RC, Proctor EK. Infusing science into politics and policy: the importance of legislators as an audience in mental health policy dissemination research. Adm Policy Mental Health. (2017) 44:160–3. doi: 10.1007/s10488-016-0752-3
26. Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. (2015) 10:21. doi: 10.1186/s13012-015-0209-1
27. Kim B, McCullough MB, Simmons MM, Bolton RE, Hyde J, Drainoni M-L, et al. A novel application of process mapping in a criminal justice setting to examine implementation of peer support for veterans leaving incarceration. Health Justice. (2019) 7:3. doi: 10.1186/s40352-019-0085-x
28. D'Andreamatteo A, Ianni L, Lega F, Sargiacomo M. Lean in healthcare: a comprehensive review. Health Policy. (2015) 119:1197–209. doi: 10.1016/j.healthpol.2015.02.002
29. FEMA. Incident Command System Resources. (2018). Available online at: https://training.fema.gov/emiweb/is/icsresource/ (accessed April 11, 2020).
31. NAACP. Ten Equity Implications of the Coronavirus COVID-19 Outbreak in the United States. National Association for the Advancement of Colored People (2020).
32. HIP. Taking Action for Health, Justice, and Belonging in the Age of COVID-19. (2020). Available online at: https://medium.com/@HumanImpact_HIP/taking-action-for-health-justice-and-belonging-in-the-age-of-covid-19-bb6b84648d98 (accessed April 13, 2020).
33. NLIHC. Coalition Hosts National Call on Needs of People Experiencing Homelessness and Others Precariously Housed During Public Health Crisis. (2020). Available online at: https://nlihc.org/news/coalition-hosts-national-call-needs-people-experiencing-homelessness-and-others-precariously (accessed April 13, 2020).
34. Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Network Open. (2020) 3:e2016938. doi: 10.1001/jamanetworkopen.2020.16938
35. COVID-19: protecting health-care workers. Lancet. (2020) 395:922. doi: 10.1016/S0140-6736(20)30644-9
36. Minder R, Peltier E. Virus Knocks Thousands of Health Workers Out of Action in Europe. The New York Times (2020). (accessed March 25, 2020). Available online at: https://www.nytimes.com/2020/03/24/world/europe/coronavirus-europe-covid-19.html
37. Stein S. CDC States How, When Health Workers With Covid-19 Can Be on Duty. Bloomberg Law (2020) (accessed April 9, 2020). Available online at: https://news.bloomberglaw.com/health-law-and-business/cdc-states-how-when-health-workers-with-covid-19-can-be-on-duty
38. Baird RP. Why Widespread Coronavirus Testing Isn't Coming Anytime Soon. The New Yorker (2020) (accessed March 24, 2020). Available online at: https://www.newyorker.com/news/news-desk/why-widespread-coronavirus-testing-isnt-coming-anytime-soon
39. Hong N. Volunteers Rushed to Help New York Hospitals. They Found a Bottleneck. The New York Times (2020) (accessed April 7, 2020). Available online at: https://www.nytimes.com/2020/04/08/nyregion/coronavirus-new-york-volunteers.html
40. Bedford T, Greninger AL, Roychoudhury P, Starita LM, Famulare M, Huang M-L, et al. Cryptic transmission of SARS-CoV-2 in Washington State. medRxiv. (2020). doi: 10.1101/2020.04.02.20051417. [Epub ahead of print].
41. COVID I, Murray CJ. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. MedRxiv. (2020). doi: 10.1101/2020.03.27.20043752
42. Ferguson N, Laydon D, Nedjati-Gilani G, Imai N, Ainslie K, Baguelin M, et al. Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality Healthcare Demand. Imperial College COVID-19 Response Team (2020).
43. Thakkar N, Burstein R, Hu H, Selvaraj P, Klein D. Social Distancing and Mobility Reductions have Reduced COVID-19 Transmission in King County, WA. Institute for Disease Modeling (2020).
44. Liu N, Stone PW, Schnall R. Impact of mandatory HIV screening in the emergency department: a queuing study. Res Nurs Health. (2016) 39:121–7. doi: 10.1002/nur.21710
45. Lee BY, Wedlock PT, Mitgang EA, Cox SN, Haidari LA, Das MK, et al. How coping can hide larger systems problems: the routine immunisation supply chain in Bihar, India. BMJ Global Health. (2019) 4:e001609. doi: 10.1136/bmjgh-2019-001609
46. Ottih C, Cussen K, Mustafa M. Building strong health supply chain systems: the visibility and analytics network approach to improving the Nigeria immunisation supply chain. BMJ Health Care Inform. (2018) 25:199–206. doi: 10.14236/jhi.v25i4.944
47. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. (2009) 4:50. doi: 10.1186/1748-5908-4-50
Keywords: implementation science, COVID-19, public health response, novel coronavirus, SARS-CoV-2
Citation: Means AR, Wagner AD, Kern E, Newman LP and Weiner BJ (2020) Implementation Science to Respond to the COVID-19 Pandemic. Front. Public Health 8:462. doi: 10.3389/fpubh.2020.00462
Received: 14 May 2020; Accepted: 23 July 2020;
Published: 02 September 2020.
Edited by:
Marcelo Demarzo, Federal University of São Paulo, BrazilReviewed by:
Elvin Hsing Geng, Washington University School of Medicine, United StatesLindsey Zimmerman, Veterans Health Administration (VHA), United States
Copyright © 2020 Means, Wagner, Kern, Newman and Weiner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anjuli D. Wagner, anjuliw@uw.edu
†These authors share first authorship
 Arianna Rubin Means
Arianna Rubin Means Anjuli D. Wagner
Anjuli D. Wagner Eli Kern
Eli Kern Laura P. Newman1,3
Laura P. Newman1,3 Bryan J. Weiner
Bryan J. Weiner